There is still no uniformly defined standard therapy for scar treatment, and various non-invasive and/or invasive methods are often used. The respective effectiveness is assessed differently depending on the indication and is dependent on several factors.
Scars are characterized by a great variability and the pathomechanism is still not fully understood [1]. Restoration of the original condition of the skin is still hardly possible; reduction of symptoms (e.g. itching, pain, contractures) as well as improvement of aesthetic aspects are considered as success criteria of a treatment [1].
Criteria-guided therapy selection
There is no standard treatment; combination therapies are often indicated [1,13]. The currently available treatment spectrum includes several options that vary in terms of invasiveness and combination possibilities [1]. Criteria for the selection of the appropriate treatment method are scar type, localization, scar size, symptomatology, clinic, duration of the condition, and medical history [1].
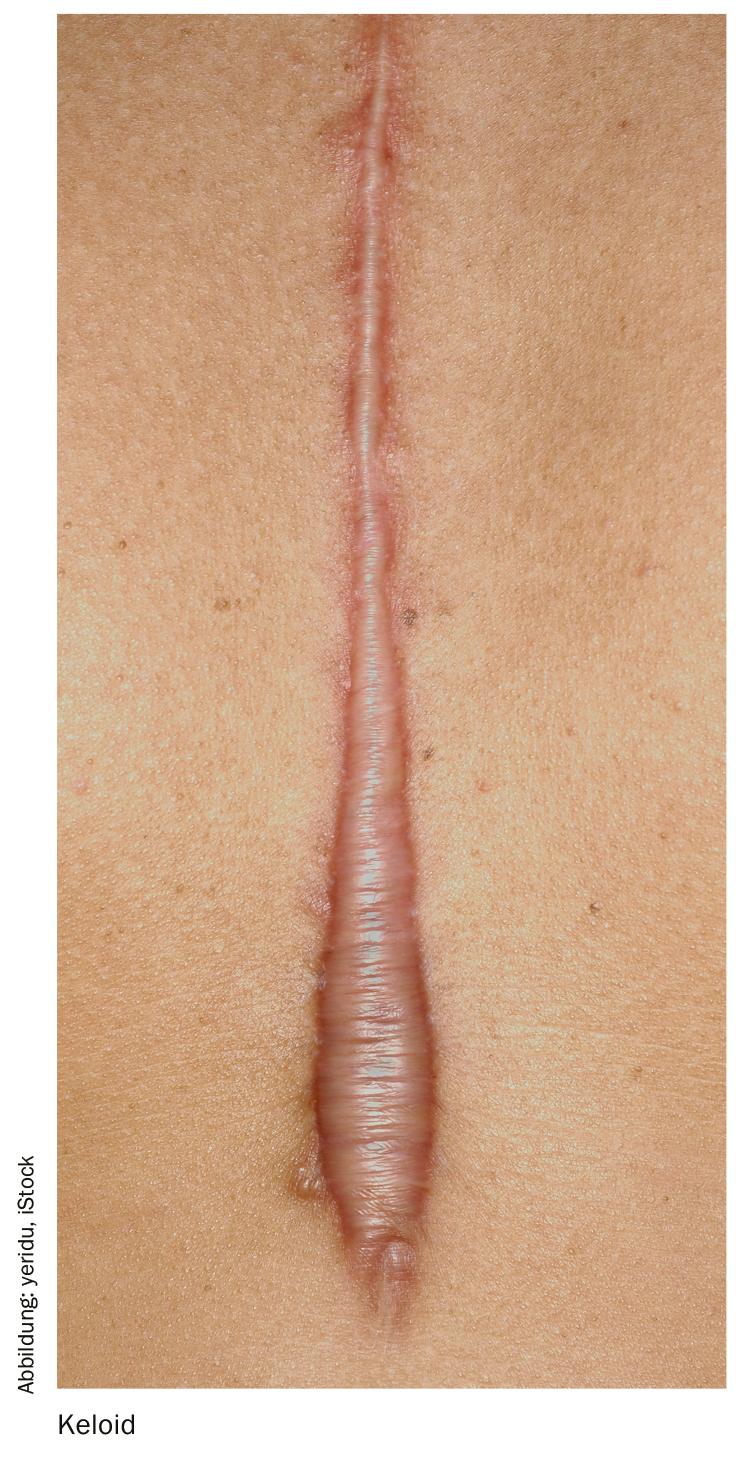
In addition to laser therapy and excision, numerous noninvasive treatment options exist, including topical topical topicals containing the active ingredients Extractum allii cepae (box), allantoin, and heparin. A single recipe for success in scar treatment does not exist; an appropriate multimodal combination of therapeutic options is advised in coordination with the time course (inflammatory/proliferative/reconstructive phase) and the phases of the wound healing process (exudative/resorptive/reparative phase; re-epithelialization; wound contraction) [1,4]. The most accurate diagnostic determination of scar type as a basis for therapy is important, but may prove difficult clinically [1]. A classification into scar types according to S2k guideline is as follows [2,3]: immature scars, mature scars, linear hypertrophic scars, areal hypertrophic scars, keloids and atrophic scars. Itching and pain are typical symptoms of many of these scar types [3].
Currently, the following treatment options are available [1,2]:
Glucocorticoids are suggested for therapy of hypertrophic scars and keloids (can be combined with cryotherapy) and for postoperative therapy of keloids. Use may be considered for postoperative prophylaxis in high-risk/predisposed patients. It is one of the best established treatment options; the success rate is up to 50-100%. In addition to anti-inflammatory effects, excessive scar growth is reduced by decreasing collagen synthesis, and glucosaminoglycan synthesis and fibroblast proliferation are inhibited. A disadvantage of this option is that the injections are painful and atrophies of the subcutis are possible if the injection is too deep, and teleangiectasias and pigmentary disorders if the injection is too superficial.
Cryotherapy is considered adequate for the treatment of hypertrophic scars and keloids and for postoperative therapy in individual cases. Use is not recommended for postoperative prophylaxis in high-risk/predisposed patients. The cold is produced by icing with liquid nitrogen, which is applied by spraying, contact or intralesional application. It is also an established procedure with proven efficacy and low recurrence rate. Adverse effects include depigmentation, pain and blistering with subsequent wound healing problems or superficial infections.

Surgical intervention for the treatment of hypertrophic scars and keloids is assessed differently depending on the type, duration and disfigurement of the scar: If hypertrophic scars are involved, treatment <1 year is not considered advisable, except with tension (e.g., plastic surgery or cosmetic disfigurement). If keloids are involved, primary surgical therapy is considered appropriate after conservative therapies have been exhausted, except in cases of narrow-based keloids or small, cosmetically disturbing keloids due to impaired wound healing. Operations are usually performed under local anesthesia or tumescent local anesthesia (TLA). In the context of postoperative therapy of keloids, use should be only complementary (supplementary to triamcinolone intralesional, pressure treatment, radiotherapy, cryotherapy). Surgical excision is classified as the ultima ratio of scar treatment and should not be used as monotherapy due to the risk of recurrence (e.g., in combination with triamcinolone).
Ablative laser treatment can be performed byCO2 laser or Er:YAG laser and is suitable for therapy of hypertrophic scars and keloids in inactive scars with contour disorders. One goal is planarization of the exophytic scar tissue. CO2 keloid ablation as monotherapy is not recommended. For narrow-based keloids,CO2 ablation in combination with adjuvant therapies is advocated. Possible side effects may include erosions, oozing, crusting, erythema, and bacterial superinfection.
For non-ablative laser treatment, an FPDL laser device (585 or 595 nm) can be used. Photothermolysis induces selective destruction of microvascularization in scar tissue, resulting in coagulation necrosis of vessels and reduction of pathological scars (via hypoperfusion and hypoxia). Non-ablative laser procedures are recommended for the therapy of hypertrophic scars and keloids for erythema reduction, e.g. in fresh vascularized scars. Possible side effects include purpura lasting about two weeks, vesicles and crusts may appear depending on the energy density used and pigmentation of the skin.
The effect of ionizing radiation (radiatio) on pathological scars is characterized on the one hand by an antiproliferative effect and on the other hand by an anti-inflammatory effect. Possible temporary side effects include redness and scaling in the radiation field, which can be treated locally using hydrating creams and photoprotection. Chronic effects such as hyper- and depigmentation, dryness of the skin, and telangiectasia depend on the total dose used (it is recommended not to exceed a total dose of 12 Gy). Irradiation is considered inappropriate for the treatment of hypertrophic scars, but adequate for keloids in individual cases. Its use is suggested for postoperative therapy in the case of keloids, but not for hypertrophic scars. For postoperative prophylaxis in high-risk/predisposed patients, this option is considered inadvisable.
Silicone gel can be considered for the therapy of hypertrophic scars and keloids as an additional therapy. For postoperative therapy as well as postoperative prophylaxis in high-risk patients/predisposition, this method is also evaluated positively. The mechanism of action of this method is not fully understood, it is believed that occlusion lead to a signaling effect to fibroblasts through cytokine release from keratinocytes. Silicone gels are a painless treatment option that is well tolerated and easy to use.
Extractum Allii cepae (Box) may be considered for the treatment of hypertrophic scars as adjunctive therapy; the use of onion extract-containing preparations for the purpose of postoperative therapy and as postoperative prophylaxis in high-risk/predisposed patients may also be considered. It is an effective, well-tolerated option.
Pressure treatment leads to a decrease in capillary perfusion, acceleration of collagen maturation and thus flattening of the scar. Adverse effects may include unpleasant sensations due to heat, sweating and swelling of the extremities, eczema, pressure erosions and ulceration. Topical pressure can be used for therapy of hypertrophic scars and keloids in case of large scars and keloids or in case of special localizations (e.g. ear), for postoperative therapy there is a recommendation in case of suitable localization.
5-Fluorouracil is suitable for keloids, especially in therapy-resistant cases. There is no recommendation for use in hypertrophic scars. Use is not recommended for postoperative prophylaxis in high-risk/predisposed patients. The mechanism of action of this pyrimidine analog is inhibition of fibroblast proliferation. Possible side effects include injection pain, hyperpigmentation, skin irritation and ulceration. Contraindicated for use in anemia, leukopenia, thrombocytopenia, pregnancy, bone marrow depression, or infection).
Interferon as monotherapy is not considered advisable; in combination with trimcinolone, its use may be considered in individual cases. Interferon-α2b is injected intralesionally, usually as two applications at intervals of four to seven days. Mild flu-like symptoms, mild pain, and inflammatory reactions at the injection site may be caused. The main mechanism of action of interferon- α and interferon- γ is a reduction in collagen I/III synthesis and glycosaminoglycan production in scar-forming fibroblasts.
Source: German Wound Congress, Bremen (D)
Literature:
- Wagner JA: Therapy of pathological scars. JDDG 2013; 1610-0379/2013/1112. DOI: 10.1111/ddg.12209
- AWMF: S2k-Leitlinie: Scars (hypertrophic scars and keloids), therapy of pathological. (AWMF Register Number: 013-030), April 2012 Long version. www.amwf.org
- Poetschke J, Gauglitz GG: Current options for the treatment of pathologic scars. JDDG 2016; 14(5): 467-478.
- Denk H, et al: Inflammation and immune response. In: Böcker W, Denk H, Heitz PhU: Pathology. Munich: Urban & Fischer, 2001.
- Jenwitheesuk K, et al: Role of silicone derivative plus onion extract gel in presternal hypertrophic scar protection: a prospective randomized, double blinded, controlled trial. Int Wound J 2012; 9: 397-402.
- Maragakis M, Willital GH, Michel G, Gortelmeyer R: Possibilities of scar treatment after thoracic surgery. Drugs Exp Clin Res 1995; 21: 199-206.
- Chung VQ, Kelley L, Marra D, Jiang SB: Onion extract gel versus petrolatum emollient on new surgical scars: prospective double-blinded study. Dermatol Surg 2006; 32: 193-197.
- Koc E, Arca E, Surucu B, Kurumlu Z: An open, randomized, controlled, comparative study of the combined effect of intralesional triamcinolone acetonide and onion extract gel and intralesional triamcinolone acetonide alone in the treatment of hypertrophic scars and keloids. Dermatol Surg 2008; 34: 1507-1514.
- Tarvady S, Anguli VC, Pichappa CV: Effect of heparin on wound healing. J Biosci 1987; 12: 33-40.
- Araújo LU, et al: Profile of wound healing process induced by allantoin. Acta Cir Bras 2010; 25: 460-466.
- Prager W, Gauglitz GG: Effectiveness and Safety of an Overnight Patch Containing Allium cepa Extract and Allantoin for Post-Dermatologic Surgery Scars. Aesthetic Plast Surg 2018; 42(4): 1144-1150.doi: 10.1007/s00266-018-1172-4
- Ocampo-Candiani J, et al: The prophylactic use of a topical scar gel containing extract of Allium cepae, allantoin, and heparin improves symptoms and appearance of cesarean-section scars compared with untreated scars. J Drugs Dermatol 2014; 13(2): 176-182.
- Nast A, et al: German S2k guideline on the therapy of pathological scars (hypertrophic scars and keloids). J Dtsch Dermatol Ges 2012; 10: 747-762.
- Fischer S, et al: Topical externals for prevention and therapy of hypertrophic scars and keloids: a literature review. Handchir Microchir plast Chir 2015; 47(04): 253-267. DOI: 10.1055/s-0035-1549919.
HAUSARZT PRAXIS 2019; 14(6): 21-22 (published 5/24/19, ahead of print).
DERMATOLOGY PRACTICE 2019; 29(3): 38-39











