Until the individually appropriate disease-modifying therapy (DMT) is available, there are
in the absence of predictive biomarkers, stepwise optimizations are often necessary, possibly resulting in multiple changes of DMT. To reduce the risk of rebound effects, a strategy for follow-up treatment should be established before discontinuation as a precautionary measure.
The heterogeneity of multiple sclerosis (MS) and the availability of different disease modifying therapies (DMTs) presents a challenge in therapy selection. The goal is to select the treatment that best meets the individual needs of the patient, taking into account efficacy and an acceptable risk-benefit ratio [1].
Therapy changes are common
Reasons for switching a DMT may include lack of efficacy, adverse events, and inadequate treatment adherence. A multicenter, retrospective Italian study analyzed data from 2954 patients newly diagnosed with relapsing-remitting multiple sclerosis (RRMS) from 2010 to 2017 [2,3]. It was found that 48% of patients had changed therapy within 3 years [2,3]. Approximately one-tenth of patients who discontinue treatment with fingolimod due to side effects or inadequate control of MS disease activity experience increased disease activity (so-called rebound) two to four months after discontinuation [4]. Therefore, as a precautionary measure, a strategy for follow-up treatment should be established before discontinuation. Fingolimod has been approved in Switzerland since 2011 for the treatment of patients with RRMS to reduce relapse frequency and delay progression of disability. Sphingosine-1-phosphate receptor modulator (S1PR) selectively and reversibly retains lymphocytes in lymph nodes, allowing important immune functions to be maintained and patients to be treated flexibly.
Study on switching from fingolimod to ocrelizumab or natalizumab
A recent study in the Journal of Neurology, Neurosurgery and Psychiatry published study led by researchers at Monash University found that the number of relapses in patients with RRMS was well controlled and disability stabilized or improved when patients who discontinued fingolimod were switched to either ocrelizumab or natalizumab [5]. First author and biostatistician Dr. Chao Zhu used a sophisticated statistical approach in his data analysis. In summary, ocrelizumab performed best in reducing the annualized relapse rate, followed by natalizumab and cladribine. Natalizumab led to the most improvements in disability, and patients remained on ocrelizumab the longest. The results at a glance:
- A total of 1 045 patients switched from fingolimod to ocrelizumab (n=445), cladribine (n=76), or natalizumab (n=524).
- The annualized relapse rate (ARR) for ocrelizumab was 0.07, for natalizumab 0.11, and for cladribine 0.25.
- Compared with natalizumab, the ARR ratio (95% confidence interval was [KI]) for ocrelizumab was 0.67 (0.47-0.96) and for cladribine was 2.31 (1.30-4.10); the hazard ratio (95% CI) for time to first relapse was 0.57 (0.40-0.83) for ocrelizumab and 1.18 (0.47-2.93) for cladribine.
- Ocrelizumab users had an 89% lower dropout rate (95% CI: 0.07-0.20) than natalizumab, but also a 51% lower likelihood of confirmed disability improvement (95% CI: 0.32-0.73).
- There was no difference in the accumulation of impairment.
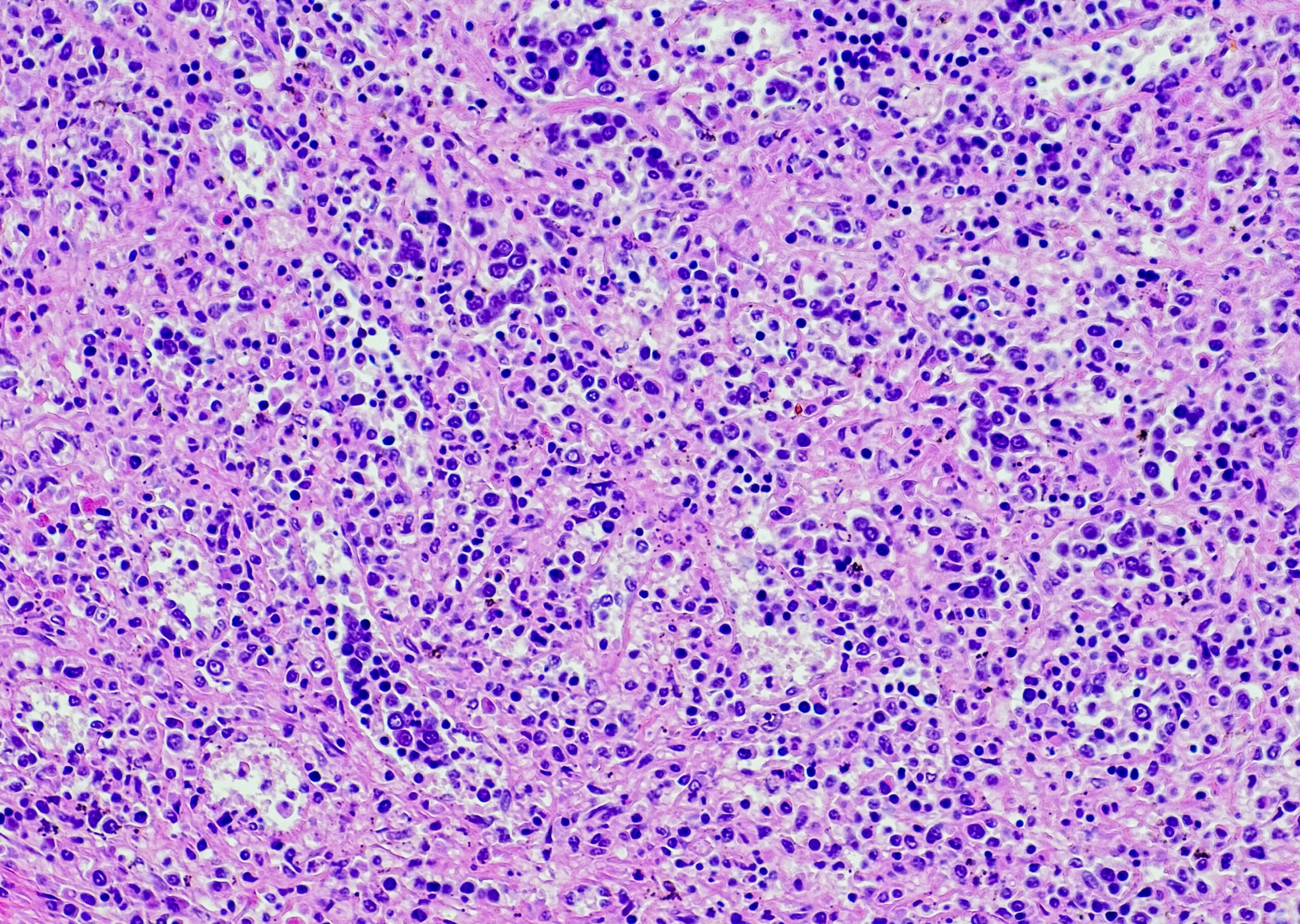
Natalizumab is a humanized IgG4 monoclonal antibody that prevents leukocyte migration into inflammatory tissues by binding to the α4-subunit of human integrins [6]. Ocrelizumab is a recombinant humanized monoclonal antibody that selectively depletes CD20-positive B cells [7].
Literature:
- Grand’Maison F, et al: Sequencing of disease-modifying therapies for relapsing-remitting multiple sclerosis: a theoretical approach to optimizing treatment. Curr Med Res Opin 2018; 34(8): 1419-1430.
- Saccà F, et al: Determinants of therapy switch in multiple sclerosis treatment-naive patients: A real-life study. Mult Scler 2019; 25(9): 1263-1272.
- Wiendl H, et al; The Multiple Sclerosis Therapy Consensus Group (MSTKG): Position paper on course-modifying therapy for multiple sclerosis 2021 (white paper) Nervenarzt 2021; 92(8): 773-801.
- Multiple Sclerosis Competence Network, Patient information on treatment with Gilenya®, www.kompetenznetz-multiplesklerose.de, (last accessed 12/12/2022).
- Zhu C, et al; MSBase Study Group: Comparing switch to ocrelizumab, cladribine or natalizumab after fingolimod treatment cessation in multiple sclerosis. J Neurol Neurosurg Psychiatry 2022; 93(12): 1330-1337.
- Delbue S, Comar M, Ferrante P: Natalizumab treatment of multiple sclerosis: new insights. Immunotherapy 2017; 9: 157-171.
- Hoffmann O, Gold R: Disease-modifying therapy of secondary progressive multiple sclerosis. Neurologist 2021; 92(10): 1052-1060.
HAUSARZT PRAXIS 2023; 18(1): 38