SGLT2 inhibitors and GLP1 receptor agonists have emerged as the drugs of first choice in the guidelines for type 2 diabetes. Sulfonylureas and insulin, on the other hand, were deprioritized due to their lower efficacy and the risk of hypoglycemia – especially in older people. Nevertheless, these drugs appear to be used more frequently, especially in older people.
Large studies on cardiovascular outcomes have demonstrated the benefit and safety of GLP1 receptor agonists and SGLT2 inhibitors, but older patients are often less represented in these studies (average age 62 to 66 years). Treatment to lower blood glucose levels should also be individually adjusted according to age-related factors (e.g. general state of health, risk of adverse events, duration of illness, life expectancy, specific concomitant diseases such as kidney and cardiovascular diseases). Some studies have also shown that some older patients may be treated too intensively with high-risk drugs such as sulphonylureas or insulin. Against this background, Danish scientists have hypothesized that older patients are increasingly being treated with high-risk drugs and less with new drugs to lower blood glucose levels.
In their register-based study, the researchers focused on patients from Denmark who were hospitalized in the period 2019 to 2020.
- used glucose-lowering medication (not insulin),
- have been diagnosed with type 2 diabetes or
- >1 consecutive HbA1c measurement >48 mmol/mol (>6.5%).
The first HbA1c measurement of each patient was used as a basis and the values were then followed for six months and examined with regard to medication use, explained Dr. Karl Sebastian Johansson, Department of Clinical Pharmacology, Bispebjerg Hospital, Copenhagen [1].
Older people treated less frequently with GLP1-RA and SGLT2 inhibitors
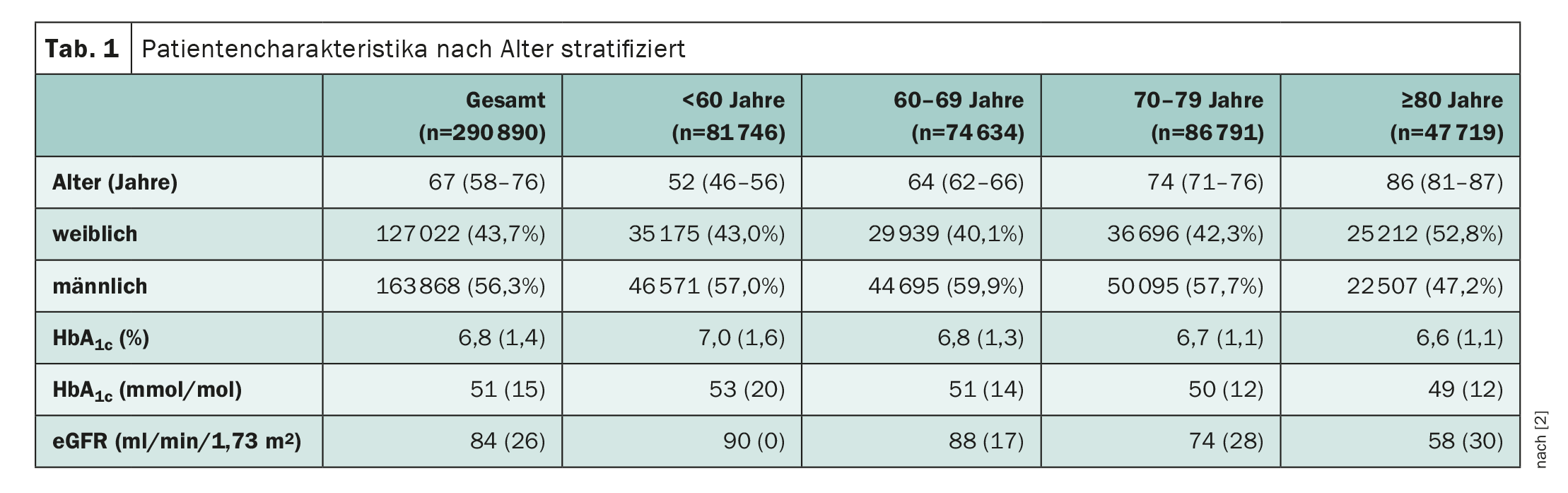
Almost 300,000 patients with type 2 diabetes (n=290,890) were included in the study. Around 47,000 participants were over 80 years old. The covariates differed according to age, with the proportion of women in the oldest age group being significantly higher than in the general age group (Table 1) . Similarly, HbA1c and renal function, as measured by eGFR, were significantly lower in the oldest group than in the youngest group. This tendency could also be seen in other covariates such as ischemic heart disease or heart failure or cancer, which were more common in the oldest age group. Socio-economic factors such as level of education, income, country of birth or treatment in primary or secondary care also differed. “All these covariates could distort our results if we end up only being interested in age,” Dr. Johanssen pointed out.
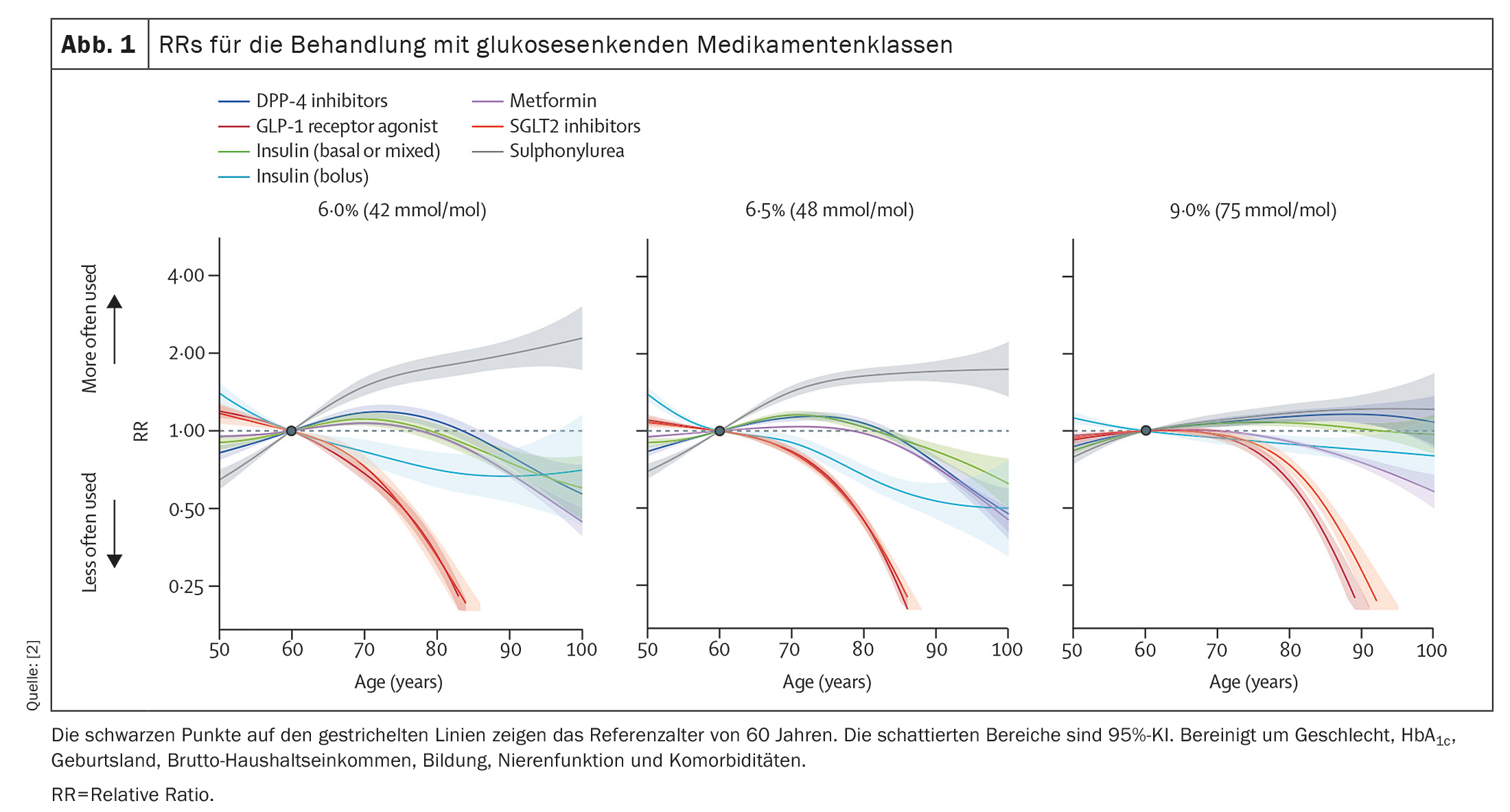
The number of medications taken peaked at the age of 70, after which it declined. When comparing 80- and 90-year-old patients with 50-year-old patients with an Hba1c value of 48 mmol/mol (6.5%), the 80-year-olds took 5% less glucose-lowering medication and 90-year-old patients took 31% less glucose-lowering medication. Older patients were generally treated less frequently with GLP1-RA and SGLT2 inhibitors. In contrast, they received insulin, dipeptidyl peptidase 4 (DPP4) inhibitors and sulfonylureas more frequently. These discrepancies were reduced with increasing Hba1c. For example, an 80-year-old patient with an Hba1c value of 48 mmol/mol (6.5%) compared to a 50-year-old patient was 59% less likely to use either a GLP1-RA or an SGLT2 inhibitor (RR 0.41, 95% CI 0.38-0.44), but 137% more likely to use sulfonylureas (RR 2.37, 95% CI 2.19-2.58) (Fig. 1).
Evaluate medication regularly according to the latest standards
Using their model, the Danish researchers were also able to calculate that the probability of receiving sulfonylureas increases with age. “If you are 80 years old, the probability of being treated with sulfonylureas is 65% higher than for 60-year-old patients. With GLP1 receptor agonists, the probability of being treated with these drugs is 55% lower at the age of 80,” says Dr. Johanssen. The same applies to SGLT2 inhibitors. With DPP4 inhibitors, metformin and insulin, there is a slight increase between the ages of 60 and 80, which then falls back below an RR value of 1.
In summary, in the Danish T2D population, older patients with the same Hba1c level were treated with fewer blood glucose-lowering drugs than younger patients. Older people were also more likely to receive drugs with a higher risk of hypoglycemia, such as sulfonylureas and insulin, and less likely to receive GLP1-RA and SGLT2i. The correlation between age and the choice of blood glucose-lowering medication could possibly indicate age discrimination. The fact that some patients aged 80 years or older were taking high-risk medication to lower blood glucose levels despite having an HbA1c value of less than 6.5% (48 mmol/mol) contradicts current treatment standards. “Our results suggest a potential to improve treatment and underline the importance of regularly re-evaluating treatment to lower blood glucose levels in all patients, regardless of age, according to the most up-to-date standards in relation to the patient’s current health status,” the scientist concluded.
Congress: EASD 2023
Sources:
- Johansson KS: Presentation “Age discrepancies in the use of glucose-lowering medications: a nationwide cohort study”; EASD Congress 2023, Hamburg, 5.10.2023.
- Johansson KS, Bülow C, Jimenez-Solem E, et al: Age disparities in glucose-lowering treatment for Danish people with type 2 diabetes: a cross-sectional study between 2019 and 2020. The Lancet Healthy Longevity 2023; 4(12): e685-e692; doi: 10.1016/S2666-7568(23)00210-6.
InFo DIABETOLOGY & ENDOCRINOLOGY 2024; 1(1): 40-41 (published on 15.2.24, ahead of print)