At the annual meeting of the European Society of Cardiology (ESC) this year, in addition to the latest scientific findings, five new guidelines were presented on diabetes, acute pulmonary embolism, supraventricular tachycardia, chronic coronary syndrome, and dyslipidemia.
High blood pressure, air pollution or poor nutrition are factors that significantly increase the risk of cardiovascular events. Nearly 70% of all cardiovascular disease can be attributed to it. But that’s not all. Scientists have detected a total of 14 such influenceable risk factors. In addition to the above, these include abdominal fat, low education, tobacco use, dyslipidemia, diabetes, low grip strength, low physical activity, depression, excessive alcohol consumption, and sodium intake above 6 g per day. Preventive improvement of these points could therefore have a positive effect on the risk of heart attack and stroke.
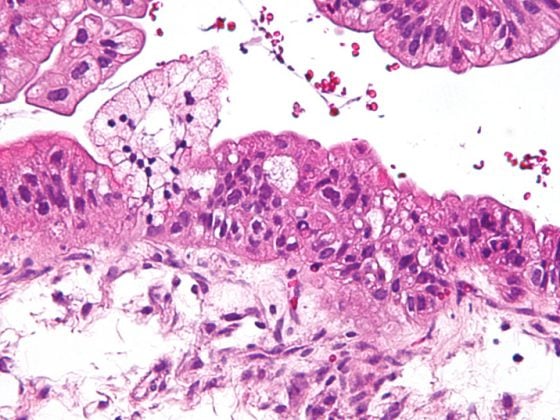
Italian researchers seem to have discovered another possible trigger for a heart attack. They compared patients with acute coronary syndrome to those with stable angina and examined the microbiome and microbes from coronary plaques. While the fecal bacteria showed mainly Bacteroidetes and Firmicutes, the coronary plaques showed mainly Proteo- and Actinobacteria. These pro-inflammatory microbes could lead to plaque rupture, which could result in vascular occlusion, according to the scientists.
New guidelines in focus
A total of five guidelines were presented on diabetes, acute pulmonary embolism, supraventricular tachycardia, chronic coronary syndrome, and dyslipidemia. The latter recommends even more aggressive reduction of LDL cholesterol to levels below 55 mg/dl for high-risk groups. These include patients with documented atherosclerotic cardiovascular disease (ASCVD) or a calculated SCORE (Systematic COronary Risk Evaluation) risk ≥10%, with familial hypercholesterolemia (FH) in combination with ASCVD or another significant risk factor, and patients with severe chronic kidney disease (eGFR <30 ml/min/1.73m2) or diabetes mellitus with end-organ damage.
Recommendations for limited exposure to air pollution and noise pollution were included for the first time in the Guidelines for Chronic Coronary Syndrome. In addition, lifestyle modification is a major focus in the management of the disease. On this point, they are consistent with the new guideline on the management of diabetes and prediabetes. Again, lifestyle modification forms an essential basis for primary prevention and dual first-line therapy in hypertension.
Oxygen does not have to be
Sour cream is routinely used in patients with myocardial infarction. But this measure does not bring much, as a large-scale study with more than 40,000 patients proves. Patients with suspected or experienced myocardial infarction were studied with respect to their 30-day mortality. It was shown that oxygen administration is neither harmful nor beneficial. The researchers therefore recommend oxygen administration only when oxygen saturation has fallen below 90%.
Detect undetected atrial fibrillation
Especially after transient ischemic attacks (TIA), in which an embolism is suspected as the causative factor, or an unclear stroke, continuous monitoring may allow conclusions to be drawn about undetected atrial fibrillation, according to the results of a registry analysis. In all 500 patients with stroke or TIA, cerebral MRI or CT imaging was suggestive of a typical thromboembolic pattern of origin. They were provided with continuous rhythm monitoring (implantable loop recorder). At 12 months, 26.8% of participants were diagnosed with atrial fibrillation. It was irrelevant whether the patients had previously suffered a stroke or a TIA.
Secondary prevention after coronary artery bypass grafting
Patient compliance with therapy after coronary artery bypass graft surgery leaves much to be desired over time. This was the conclusion of a study that examined secondary prevention in Sweden. If the medication intake was still regular in the first six months, it decreased significantly over time. After eight years, adherence was only 77.3%. However, secondary prevention is closely associated with mortality. Statins can reduce relative risk of death by 44%, platelet inhibitors by 26%, and RAAS inhibitors by 22%. Therefore, even older patients beyond 75 years of age, who have been shown to be less likely to receive secondary prevention medications, should not be treated differently from younger affected individuals.
Source: 2019 Annual Meeting of the European Society of Cardiology (ESC)
CARDIOVASC 2019; 18(5): 28 (published 10/10/19, ahead of print).