One of the therapeutic goals in ankylosing spondylitis is to reduce spinal ankylosing progression. Data from the AxSpA cohort SCQM provide further evidence regarding the efficacy of TNF inhibitors.
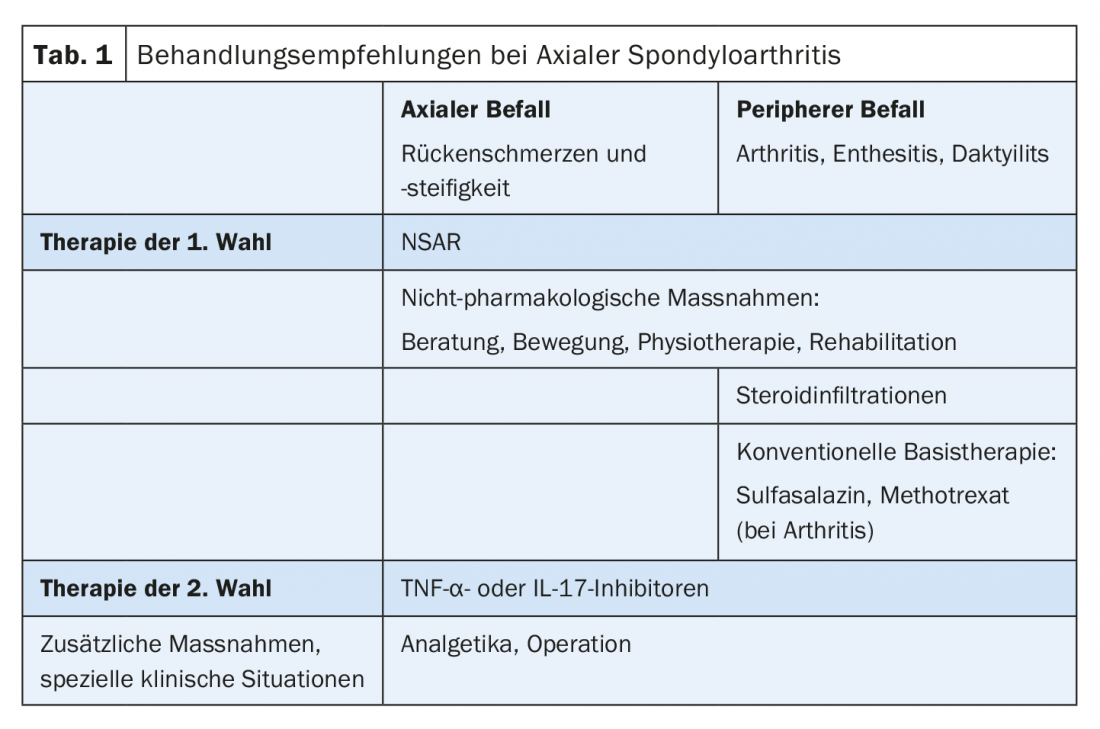
The rheumatic systemic disease ankylosing spondylitis, a form of axial spondyloarthritis (AxSpA), is characterized by chronic inflammatory, seronegative processes. The caudal spine and sacroiliac joints are mostly affected. In the case of axial involvement, which manifests as back pain and stiffness, treatment initially focuses on the administration of NSAIDs. This measure is flanked by counseling services (among others by the Swiss Bekhterev’s Disease Association, SVMB) and appropriate physical activity or physiotherapy. TNF-α or IL-17 inhibitors are used as second-line therapy (Table 1).
Can TNF blockers inhibit increasing ankylosis? “A big question in the last few years,” says PD Adrian Ciurea, MD, at the medical congress in Davos. He and his team work with data from the AxSpA cohort SCQM, the largest ankylosing spondylitis patient pool in Switzerland. For nearly two decades, TNF inhibitors have been used in ankylosing spondylitis patients with inadequate response to conventional therapies to reduce symptoms and inflammatory activity; secukinumab 150 mg was shown to be effective in two phase III RCTs [1]. In addition to inflammatory processes, spinal ankylosis also has a negative effect on the mobility and functionality of the spine. Delaying this is therefore also an important treatment goal [2].

The relationship between TNF inhibition and ankylosis was also investigated by Dr. Ciurea and his team. Their study published in 2018 [3] supported the theory that TNF blockers have a retarding effect on spinal ankylosis by reducing disease activity. Included were 432 patients from the AxSpA cohort. The follow-up of the longitudinal study was ten years with clinical and radiographic assessments every two years. Comparison between radiographic findings of patients with and without TNF inhibition showed: TNF blockers reduce the likelihood of progression in the next two years by half; progression is defined as an increase of ≥2 mSaSSS units every two years. However, to observe this effect, therapy for at least two years was required; below this time mark, no effect was seen. In addition, the longer the treatment, the greater the reduction in progression. This is – also confirmed by the study – triggered by the decrease in inflammatory activity. The authors accounted for the number of syndesmophytes, the degree of inflammation, and a male gender as predictors of progression.
The results suggest that early diagnosis and thus early initiation of therapy are important. For primary care physicians, this means working closely with rheumatologists to quickly identify patients who need biologics.
Source: 85th Medical Congress Davos, February 7-9, 2019.
Literature:
- Sepriano A, et al: Efficacy and safety of biological and targeted-synthetic DMARDs: a systematic literature review informing the 2016 update of the ASAS/EULAR recommendations for the management of axial spondyloarthritis. RMD Open 2017; 3(1): e000396.
- Poddubnyy D, Sieper J: Radiographic progression in ankylosing spondylitis/axial spondyloarthritis: how fast and how clinically meaningful? Curr Opin Rheumatol 2012; 24(4): 363-369.
- Molnar C, et al: TNF blockers inhibit spinal radiographic progression in ankylosing spondylitis by reducing disease activity: results from the Swiss Clinical Quality Management cohort. Ann Rheum Dis 2018; 77: 63-69.
HAUSARZT PRAXIS 2019; 14(3): 39-40











