The results of the prospective observational study showed that in patients over 65 years of age with atrial fibrillation, treatment with rivaroxaban was associated with a significantly increased risk of severe ischemic or hemorrhagic events compared with apixaban.
Atrial fibrillation (VHF) is the most common cardiac arrhythmia and increases the risk of stroke fivefold [1,2]. Anticoagulation is an important treatment pillar for the prevention of stroke [3]. In a retrospective analysis in elderly frail patients with VCF, the risk of stroke, embolism, and major bleeding was found to be significantly lower with treatment with direct oral anticoagulants (DOAKs) than with vitamin K antagonists [4,5]. DOAKs such as rivaroxaban and apixaban – both direct factor Xa inhibitors – are among the preferred class of agents for this patient population. Ray et al. investigated whether there is a difference in the risk of serious ischemic or hemorrhagic events depending on which of these two anticoagulants was used in patients over 65 years of age with VCF in a study published in JAMA in 2021 [5].
Comparison in favor of apixaban – even at reduced doses
The study included 581 451 patients with AF treated with either rivaroxaban or apixaban [5]. The median follow-up time was 5.8 (2.1-13.2) months. The mean age of study participants was 77.0 years and 50.2% were female. 76.9% of subjects received anticoagulation at standard doses and 23.1% at reduced doses. In the entire study population, 6946 majore ischemic or hemorrhagic events occurred during follow-up. The risk with rivaroxaban proved to be higher compared with apixaban, with adjusted rates of 16.1 vs. 13.4 per 1000 person-years (HR, 1.18; 95% CI 1.12-1.24) (Fig. 1) [5]. Both the risk of major ischemic events (HR 1.12; 95% CI 1.04-1.20) and hemorrhagic events (HR 1.26; 95% CI 1.16-1.36) were increased with treatment with rivaroxaban [5].
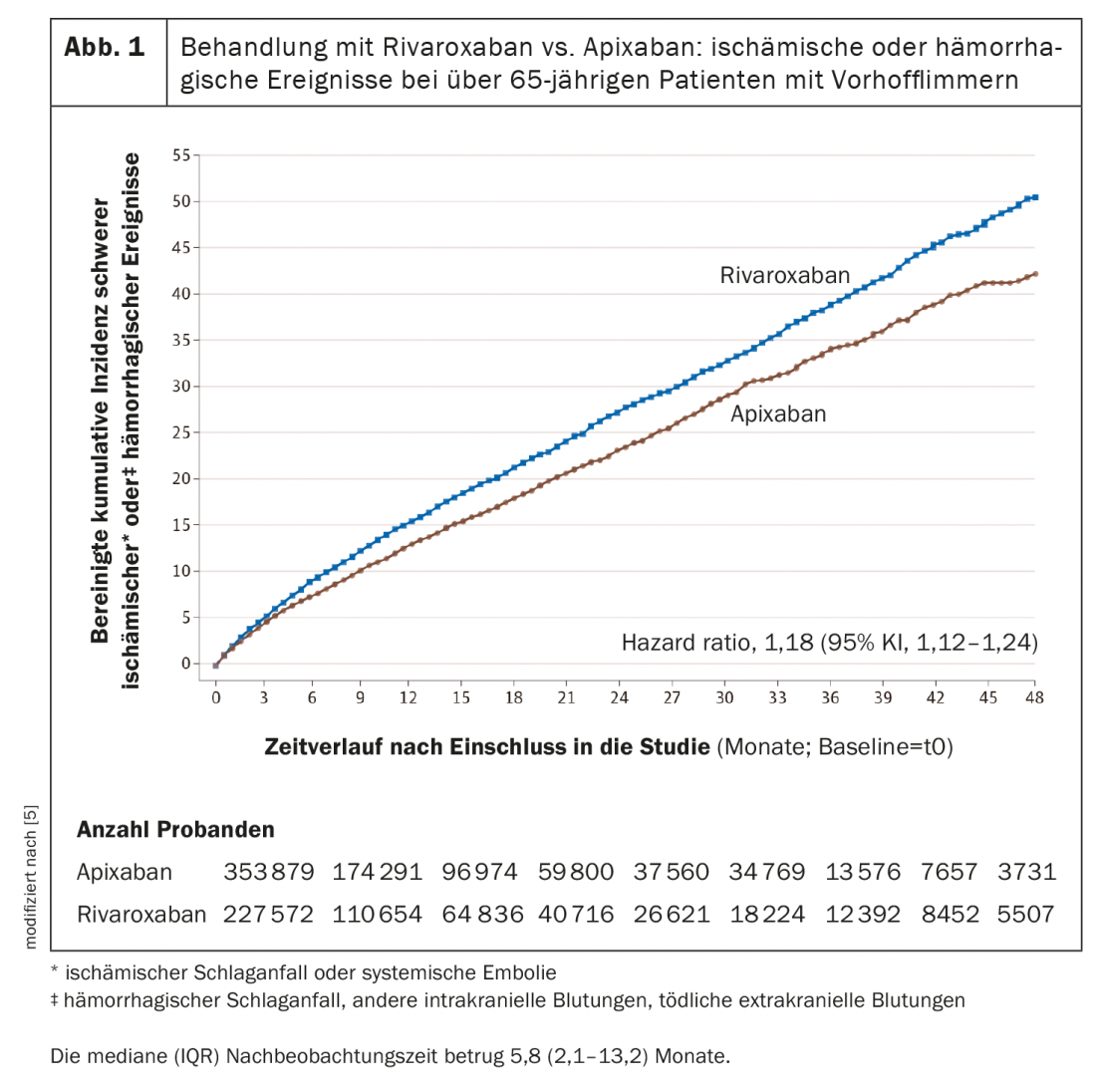
DOAK treatment was started at reduced doses in 23% of study participants in each group, for a total of 134,393 patients [5]. Also in this patient population, a difference in favor of apixaban was manifested, respectively, the risk for ischemic and hemorrhagic events was increased under rivaroxaban. Patients receiving DOAKs at reduced doses had a higher mean age compared with those receiving standard doses (82.8 vs 75.2 years). In addition, the prevalence of other risk factors for bleeding or stroke was higher (mean CHA2DS2-VASc score, 5.0 vs. 4.1).
Practice-relevant expansion of the evidence base
Although the efficacy of rivaroxaban and apixaban in VCF has been compared in previous retrospective cohort studies [6–8], the present data produced new insights that are very valuable for clinical practice. With more than half a million new users of rivaroxaban or apixaban, this was a larger cohort than in previous studies. Furthermore, only patients over 65 years of age were included [9,10]. The larger sample size allowed more accurate quantification of the occurrence of rare but clinically important events, such as fatal extracranial hemorrhage. In contrast to other studies, patients receiving reduced-dose oral anticoagulation were also included, a subpopulation of VHF sufferers that is particularly vulnerable because of common patient characteristics [5–7].
Literature:
- Singer E, et al: Medicine and Reason 2015; 3-82.
- Zimetbaum P: Ann Intern Med 2017; 166(5): ITC33-ITC48. doi:10.7326/AITC201703070
- January CT, et al: Circulation 2019; 140(2):e125-e151.
- Lip GYH, et al: J Intern Med 2020; https://doi.org/10.1111/JOIM.13140
- Ray WA, et al: JAMA. 2021 Dec 21; 326(23): 2395-2240.
- Graham DJ, et al: Am J Med 2019; 132(5): 596-604.e11.
- Fralick M, et al: Ann Intern Med 2020; 172(7): 463-473.
- Lip GYH, et al: Stroke 2018; 49(12): 2933-2944.
- Go AS, et al: JAMA 2001; 285 (18): 2370-2375.
- Lowenstern A, et al: Ann Intern Med. 2018;169(11): 774-787.
HAUSARZT PRAXIS 2022; 17(5): 32