There is a lot happening in the landscape of hematologic neoplasms. This year, several potentially standard-changing studies could be presented to Congress at . Fitting to the claim of the annual congress of the European Hematology Association, which aims to bring state-of-the-art evidence-based approaches to diagnosis and therapy as well as the latest developments from research into practice.
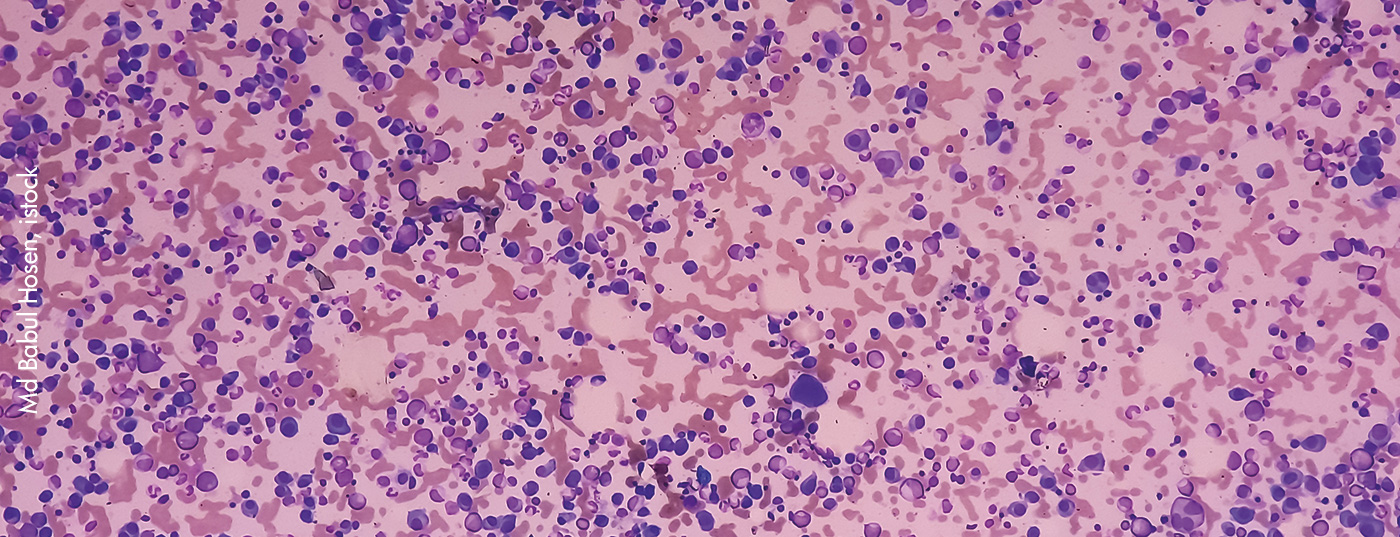
30 years of EHA were celebrated in a very special way this year. Especially in the field of hematologic neoplasms, some groundbreaking study results could be presented. Hematologic malignancies account for only about 7% of all tumors, but they continue to pose significant challenges to practitioners. Especially the very heterogeneous manifestations require an exact diagnosis as well as very specific therapy management in order to achieve the best possible prognosis for the patients. Therefore, combination treatments are increasingly used to exploit additive effects of the individual parameters.
For example, in FLT3-IDT+ acute myeloid leukemia, intensive chemotherapy in combination with quizartinib prolonged overall survival. In activated PI3Kδ syndrome, the specific PI3Kδ inhibitor leniosilib resulted in an increase in naive B lymphocytes, achieving a decrease in lymphadenopathy and cytopenia. Patients with symptomatic, treatment-naive, primary or secondary myelofibrosis benefit from therapy with the JAK1/2 inhibitor momelotinib after pretreatment with JAK inhibitors. This was able to achieve a reduction in symptomatology and spleen size, as well as an increase in transfusion independence.
Focus on multiple myeloma
Exciting study results were also presented in multiple myeloma (MM). The triple combination of lenalidomide, bortezomib, and dexamethasone (RVd) have long been the standard of care for patients with newly diagnosed MM who are eligible for transplantation. Now, combination of RVd with autologous stem cell transplantation and lenalidomide maintenance until progression was studied in more detail. It resulted in a 21.4-month increase in median progression-free survival compared with RVd alone. However, overall survival was not prolonged.
The addition of an anti-CD38 antibody to RVd looks promising. A phase III study was conducted to further elucidate the efficacy of the combination of isatuximab with RVd in induction therapy. It was investigated whether quadruple treatment could repress disease activity as much as possible and achieve the greatest MRD (measurable residual disease) negativity. Achieving MRD negativity was defined as failure to detect residual disease in the bone marrow prior to high-dose therapy followed by autologous hematopoietic stem cell transplantation. MRD negativity is an important clinical endpoint associated with improved outcome. This is especially important in the present patient clientele, who frequently relapse. It was shown that the four-agent combination resulted in a deeper response after induction and that the benefit in terms of MRD was consistent. MRD negativity rates in bone marrow after induction therapy were 50.1% versus 35.6% with RVd. A significant influence on the safety profile by the additional administration of the anti-CD38 antibody could not be detected. Rates of all observed adverse events were 63.6% for the isatuximab combination versus 61.3% for RVd, and serious adverse events and discontinuations were similar in both study arms (34.8% and 36.3%, respectively). The study will be continued with further analysis of progression-free survival after the next therapy interventions.
Comparison of therapy in Burkitt’s lymphoma
High-risk Burkitt’s lymphoma is said to occur when patients have elevated LDH levels, WHO performance status ≥2, stage III/IV, or a tumor mass at least 10 cm in diameter. The problem with this disease is that there is currently no standard of care. Ultimately, the choice is between two immunotherapies. R-CODOX-M/R-IVAC is a high-dose treatment management, whereas DA-EPOCH-R is less aggressive and thus tends to appear less effective. This assumption has now been refuted in a direct comparison. Dose-adapted EPOCH-R resulted in equal remission rates and survival at two years as R-CODOX-M/R-IVAC, but was associated with fewer side effects.
Congress: EHA 2022
InFo ONCOLOGY & HEMATOLOGY 2022; 10(4): 22.