Case report: Mother presents with her 24-month-old boy. This one suffers since the sixth month of life from strongly itching nodules on the scalp and partly also on other parts of the body. These suddenly flare up at regular intervals, crust over after a few days and finally heal.
Repeated bacteriological, virological and mycological smears were inconclusive. The child is always in good general health during the episodes, and the older siblings are not affected. The previous therapies with topical, and once also systemic antibiotics have had no influence on the course of the disease.
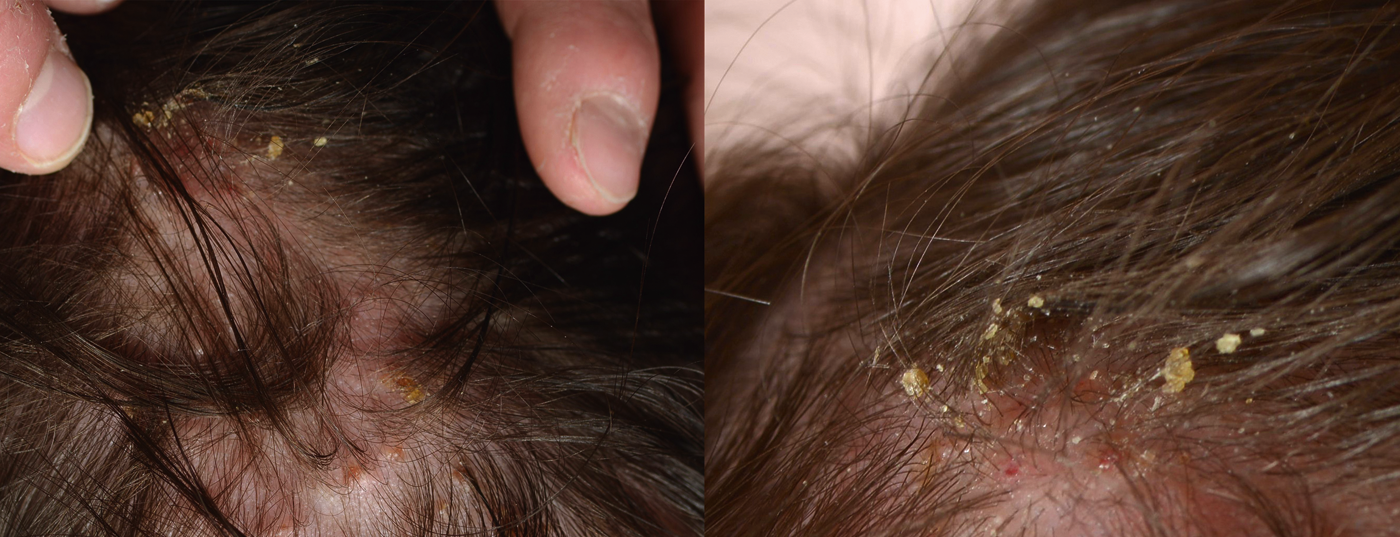
Clinical picture: Examination reveals multiple whitish to yellow, sagocorneous, partially crusted papules and pustules on the scalp (Fig. 1). In addition, multiple whitish papules and pustules, partly with erythematous, urticarial surroundings, are detectable in the area of the back ( Fig. 2).

Quiz
Based on this information, what is the most likely diagnosis?
A Recurrent pyoderma of the scalp.
B Langerhans cell histiocytosis
C Eosinophilic pustular folliculitis.
D Scabies
E Incontinentia pigmenti
Diagnosis and Discussion: This clinical presentation of recurrent, intensely pruritic papules and pustules on the capillitium and dorsum is characteristic of eosinophilic pustular folliculitis of scalp in infancy (Answer C). This subtype of eosinophilic pustular folliculitis was first described in 1984 [1] and is distinguished from classic (Ofuji) and HIV-associated eosinophilic pustular folliculitis because of its early age of manifestation and different distribution [2]. Etiology and pathogenesis are largely unknown, and associations with other diseases are not available [3]. Contrary to what is stated in the literature, in our experience it is by no means a rare clinical picture. Thus, we certainly see one affected child per month in our clinic.
Usually boys are affected for the first time in the first months of life, sometimes already at birth. Thereafter, the skin lesions occur cyclically every two to eight weeks, may involve the extremities or trunk in addition to the obligately affected capillitium, are sterile, and heal after 7-20 days with the formation of crusts [3]. The general condition is always unrestricted.
The diagnosis is usually made clinically. Pathogen-related folliculitis should be excluded in the first episode. For confirmation, multiple eosinophilic granulocytes may be detected in the pustular smear; less frequently, biopsy confirmation of the diagnosis is performed. In the blood count, peripheral eosinophilia is also frequently present in early phases. However, these further clarifications are not mandatory in the typical case.
Depending on the age of manifestation and clinical presentation, differential diagnosis may include erythema toxicum neonatorum, infections (bacteria, fungi, scabies), Langerhans cell histiocytosis, incontinentia pigmenti or, if the palmoplantar region is involved, infantile acropustulosis. The latter is also interpreted by some authors as a manifestation of the same clinical picture [4]. In addition, an eosinophilic, papulopustular eruption on the capillitium, face, and upper trunk occurring in the first weeks of life may be the initial symptom of a hyper-IgE syndrome, but later includes other symptoms such as “cold abscesses,” mucocutaneous candidiasis, sinopulmonary infections, and severely elevated total IgE [5].
Therapeutically, potent topical steroids are used, which lead to a significant shortening of the individual episodes. In very pronounced cases, systemic steroids or dapsone can also be used in the short term, but they are usually not necessary because of the benign course and the expected healing in the first three years of life.
Knowledge of this benign and typical clinical picture can play a decisive role in avoiding unnecessary investigations and reassuring parents.
Lisa Weibel, MD
Regula Wälchli, MD
Martin Theiler, MD
Literature:
- Lucky AW, et al: Eosinophilic pustular folliculitis in infancy. Pediatr Dermatol 1984; 1: 202-206.
- Nervi SJ, Schwartz RA, Dmochowski M: Eosinophilic pustular folliculitis: a 40 year retrospect. J Am Acad Dermatol 2006; 55: 285-289.
- Hernandez-Martin A, et al: Eosinophilic pustular folliculitis of infancy: a series of 15 cases and review of the literature. J Am Acad Dermatol 2013; 68: 150-155.
- Vicente J, et al: Are eosinophilic pustular folliculitis of infancy and infantile acropustulosis the same entity? Br J Dermatol 1996; 135: 807-809.
- Yong PF, et al: An update on the hyper-IgE syndromes. Arthritis research & therapy 2012; 14: 228.
DERMATOLOGIE PRAXIS 2014; 24(2): 20-21