The established cardiac markers BNP, NT-pro-BNP, troponins, and D-dimers are important diagnostic tools. However, they can be false-positive and thus lead to misdiagnosis. In a seminar at this year’s KHM Congress, Prof. Franz Eberli, MD, Zurich, explained when the determination of cardiac markers is useful and helpful, and where their limitations lie.
The natriuretic peptides (ANP, BNP, CNP, urodilatin) are very potent and have a whole range of roles such as:
- Natriuresis
- Diuresis
- Vasodilation
- Improvement of diastolic function
- (lusitropic effect)
- Inhibition of the RAA system
- (Renin-Angiotensin-Aldosterone System)
- Inhibition of endothelin release
- Inhibition of smooth muscle cell and endothelial cell growth
- Inhibition of cell division.
Enzymatic cleavage produces NT-pro-BNP and BNP from pro-BNP, which have different dynamics. NT-pro-BNP is more stable and fluctuates less than BNP, making it more suitable as a progression parameter. BNP and NT-pro-BNP levels are not elevated in noncardiac dyspnea, helping to distinguish cardiac from noncardiac dyspnea. Further, they correlate relatively well with heart failure severity and, together with clinic, increase diagnostic accuracy. Regarding rule-in and rule-out values, BNP and NT-pro-BNP have to be considered separately.
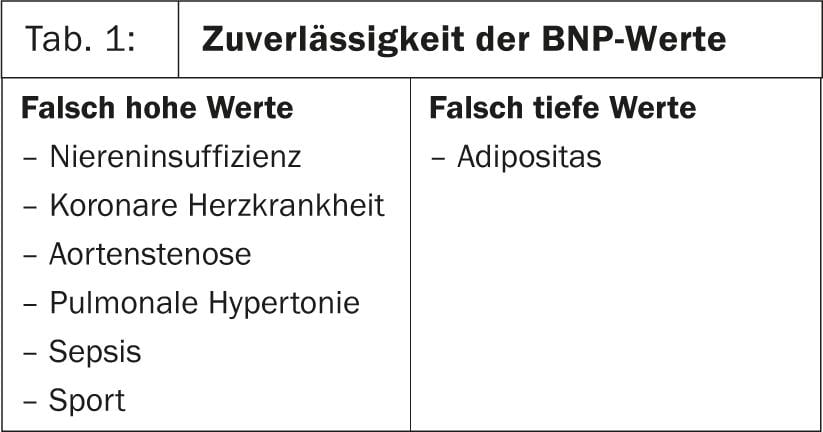
Heart failure is unlikely at a BNP <100 pg/ml and likely at >400 pg/ml. If the values are in between, the diagnosis is uncertain. When interpreting the values, it must be noted that they are elevated, for example, in renal insufficiency, but also after exercise(Table 1). “With a patient who comes to your practice on a bicycle, you cannot utilize the BNP. The resting value is only reached again after one to two hours,” emphasized Prof. Franz Eberli, MD, Zurich.
NT-pro-BNP is more stable than BNP, but it has the disadvantage that the normal values are age-dependent, unlike BNP. “This is not taken into account in the ESC guidelines or by the laboratories. In older patients, it can therefore happen that the laboratory marks a value as pathological, although it would be normal for this age group. This is misleading, and caution is required here,” warned Prof. Eberli. “Combine that with the fact that many labs no longer determine age-independent BNP but automatically provide NT-pro-BNP when you order a BNP.” Rule-in and rule-out values of NT-pro-BNP for different age groups are shown in Figure 1.

On various occasions, it has been advocated that heart failure treatment should be titrated on the basis of BNP or NT-pro-BNP levels. However, some studies have now shown that no relevant improvement can be achieved by this, at least in the older patients, which is why this procedure is not recommended.
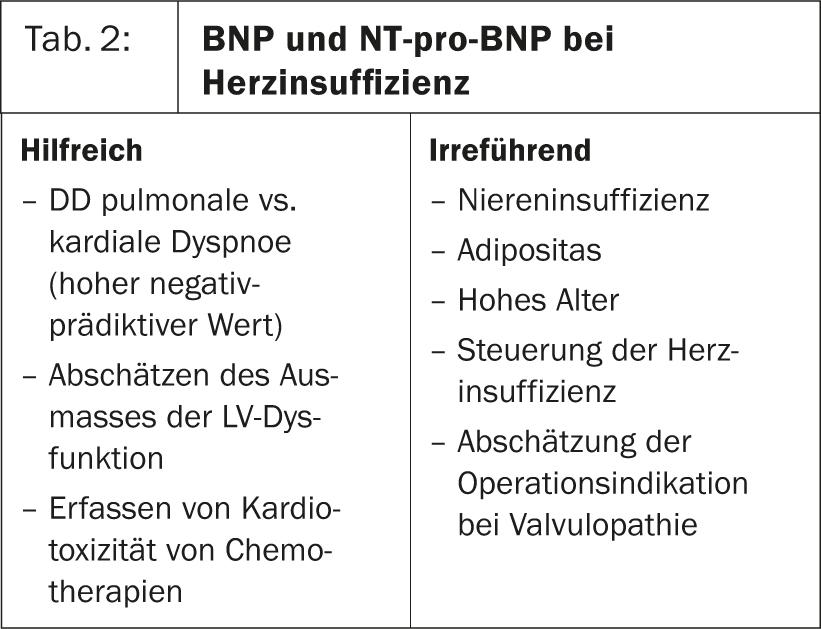
In conclusion, BNP and NT-pro-BNP are helpful in distinguishing cardiac from noncardiac dyspnea and in estimating the extent of left ventricular dysfunction. However, it is important to keep in mind that the values are elevated in renal insufficiency (the worse the kidney, the higher the values) and the normal values of NT-pro-BNP are age-dependent(Table 2).
Risk of misdiagnosis with hs-troponin
Cardiac troponins are very specific and therefore good markers that are very useful in differentiating between cardiac and noncardiac pain and in risk stratification in acute coronary syndrome (ACS) (Fig.2, Table3) . Like natriuretic peptides, troponins have a very high negative-predictive value. However, they have a limited sensitivity and rise only after 4-6 hours, which is why today more and more laboratories determine only the more sensitive hs-troponin, which rises already after 2-3 hours. “There is only one measurement method for hs-troponin, but a low level can also be detected in virtually all healthy individuals. Therefore, diagnosis becomes more complicated and there is a risk of misdiagnosis,” says Prof. Eberli. In contrast, the point-of-care tests for hs-troponin commonly used in practices are very reliable. Troponins are not suitable for follow-up assessment because they have a half-life of 2-3 days.
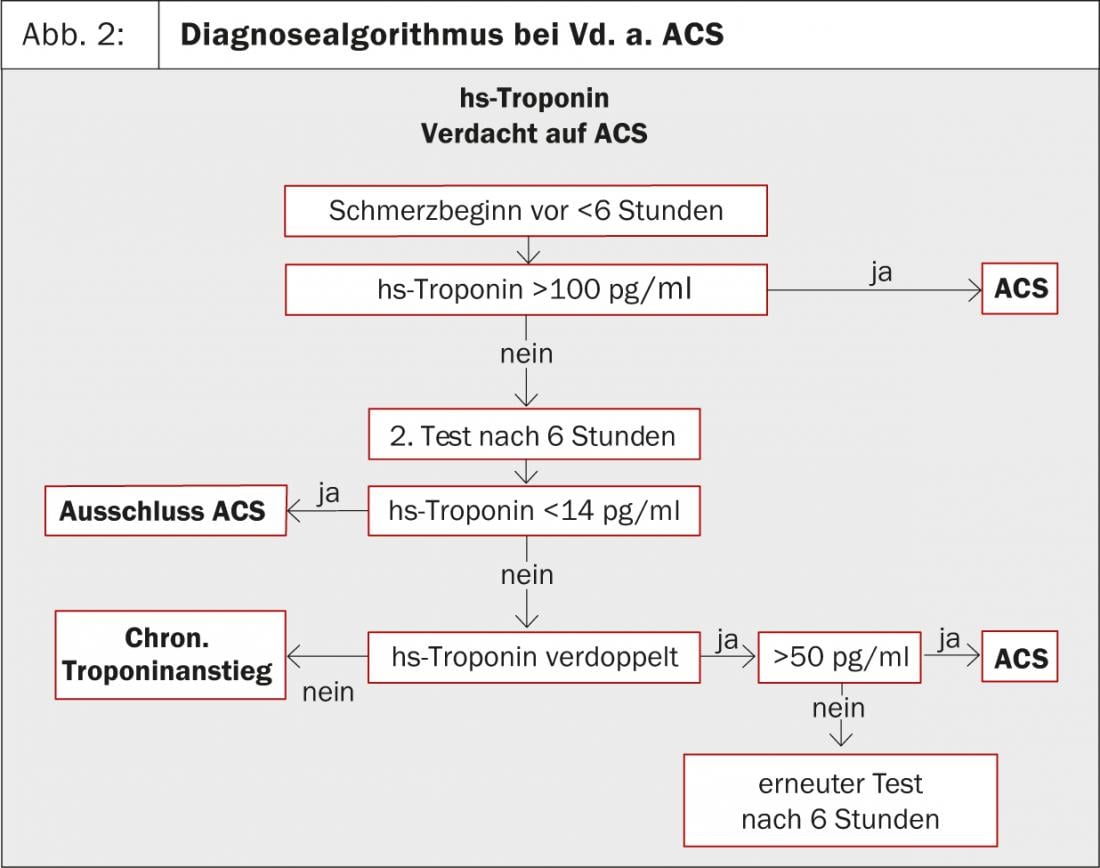
It should be further considered that troponins may also be elevated in nonischemic myocardial damage, such as myocarditis, pulmonary embolism, tachycardic atrial fibrillation, acute heart failure, pulmonary edema, or cardiac trauma, and also in renal failure, neoplasia, and rhabdomyolysis(Table 3).

D-dimer – high negative predictive value
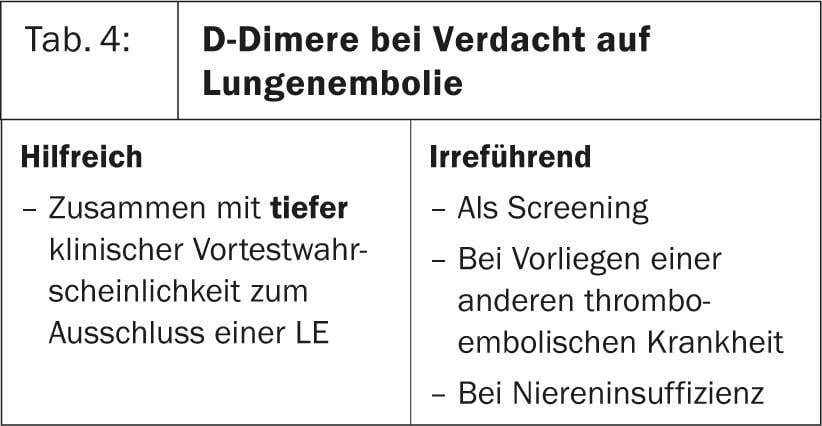
Sensitivity and specificity of clinical assessment in suspected pulmonary embolism are insufficient. Here, the determination of D-dimers can be very helpful. Depending on the assay, the determination time varies between 2 min and >8 hr, the sensitivity between 82% and 95%. “The faster the test, the worse the sensitivity,” Prof. Eberli emphasized. For D-dimers, too, there are many other reasons for elevation besides pulmonary embolism (other thromboembolic events, age >70 years of age, liver or kidney insufficiency, inflammatory condition, stress, physical exertion, surgical interventions, etc.), which is why the specificity of D-dimers is low, but the negative predictive value is very high at low clinical probability. The D-dimers are therefore particularly useful for reliably ruling out pulmonary embolism at low clinical probability (Table 4).
Source: “Cardiac markers, when helpful, when misleading?”, seminar at the 15th Continuing Education Conference of the College of Family Medicine (KHM), June 20-21, 2013, Lucerne.