In intussusception, a section of bowel is pushed into the neighboring section. This change is also known as intussusception. The intussuscepted part of the intestine is the invaginate, the receiving part of the intestine is the invaginans. The cause is often unknown.
Sudden stomach pain and intermittent, sometimes bilious vomiting, in many cases several times an hour, indicate the change. The episodes last about 15-20 minutes. In children, a relaxed posture with bent legs is noticeable.
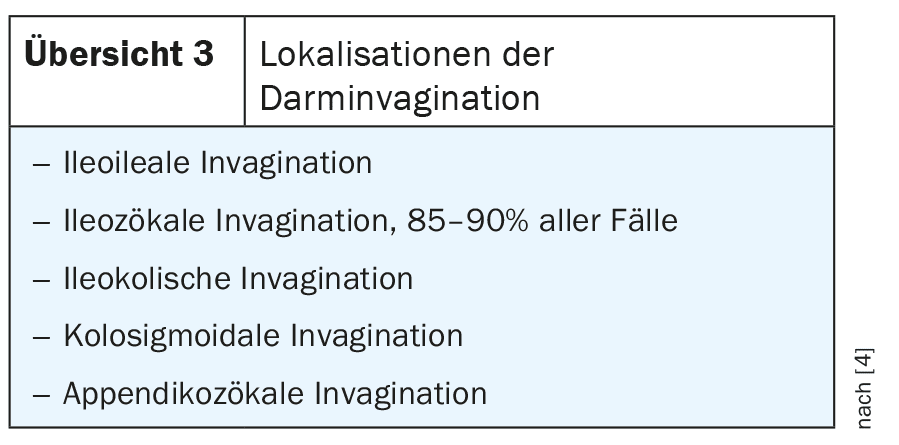
Persistent pain symptoms may indicate a developing complication. In the further course, bloody stools (“raspberry jelly”) may occur [3,4,6]. Intestinal intussusception is the most common cause of intestinal obstruction in children, especially in infants between 6 months and 3 years of age. 75% of young patients are younger than 2 years. Males are slightly more frequently affected. In about 25% of affected children, a causative pathological change triggers the intussusception (Overview 1). If spontaneous reduction does not occur, an attempt can be made to repair the bowel, for example with air insufflation (with an increased risk of bowel wall perforation) or a saline or contrast medium enema under sonographic or fluoroscopic control. The recurrence rate of manipulation is around 5 to 10%. Ultrasound monitoring should therefore be performed within 24 hours. If the reduction is unsuccessful, there is a risk of intestinal wall ischemia with subsequent gangrene and acute peritonitis. Surgical treatment is then unavoidable at the latest. The indications for surgery are summarized in Figure 2. Around 6% of intussusceptions occur in adults [5].
The intussusceptions can occur in different parts of the bowel. Overview 3 shows the different localizations.
In addition to the clinical symptoms, abdominal palpation may reveal a cylindrical tumor and rectal examination may reveal blood.
Intestinal intussusception is a possible form of intestinal displacement. Hemorrhoids can also lead to anal or rectal prolapse. The clinical diagnosis is then clear [1]. However, external colonic displacement is also possible postoperatively if an anus praeter is created.
Another form of intestinal displacement is volvulus [8]. This involves a twisting or entanglement of parts of the intestine. The consequences can be intestinal obstruction or gangrene. It is an abdominal emergency. The symptoms are similar to those of intussusception. Displacement of parts of the intestine from their normal position without volvulus can also be symptomatic if alteration of the mesentery occurs.
Sonographically, the telescope-like invagination of the affected bowel segments is very clearly visible and typical of intussusception [6]. The intussusception shows no peristalsis. In the advanced stage, vascularization decreases in Doppler ultrasonography. Sonography is also often the first imaging measure in volvulus. The radiologic abdominal overview image often shows a coffee bean-like configuration of the overinflated parts of the intestine. The distribution of air in the abdomen can also be visualized in the appropriate body position and free gastrointestinal perforations can be ruled out [7].
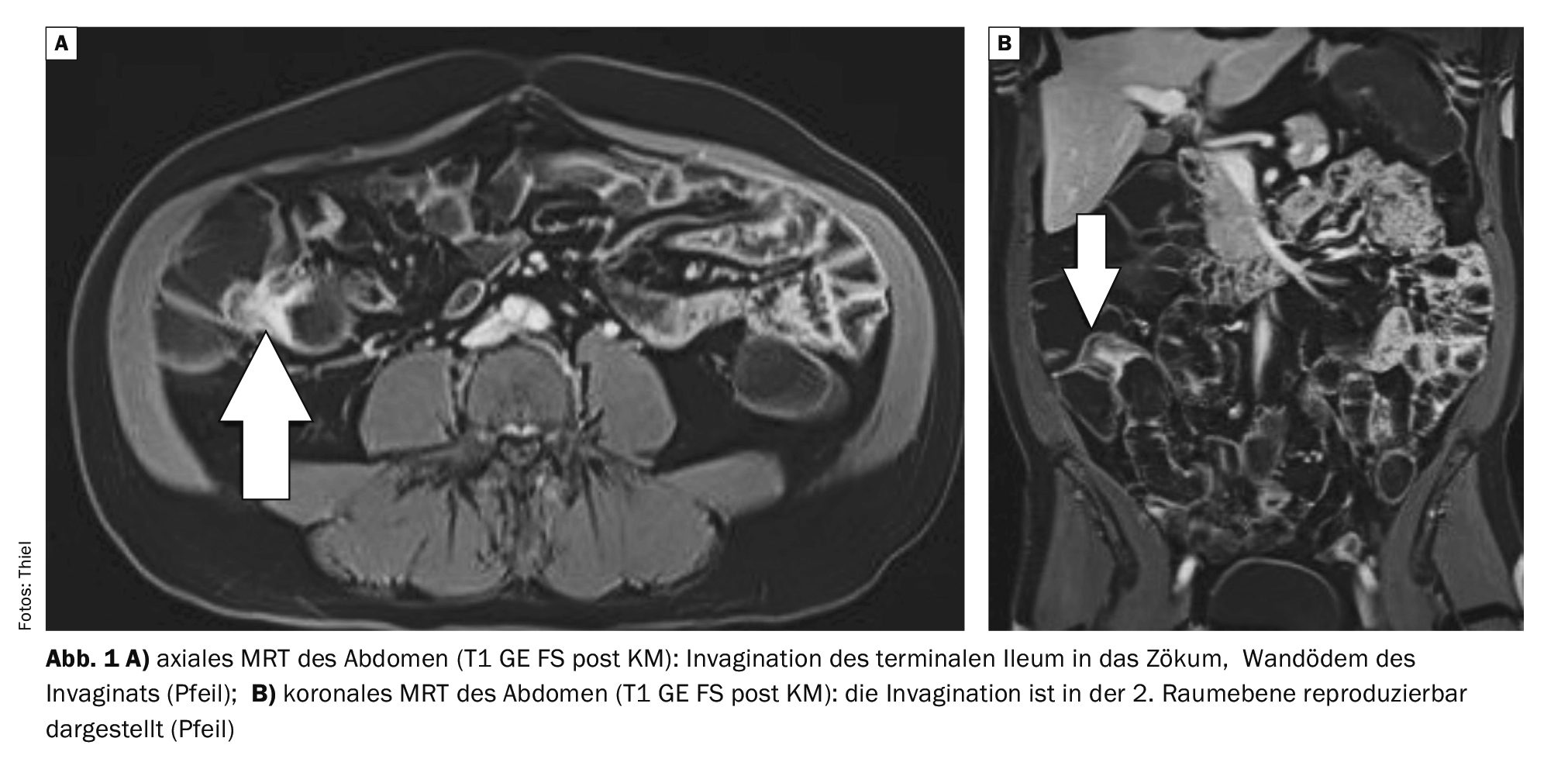
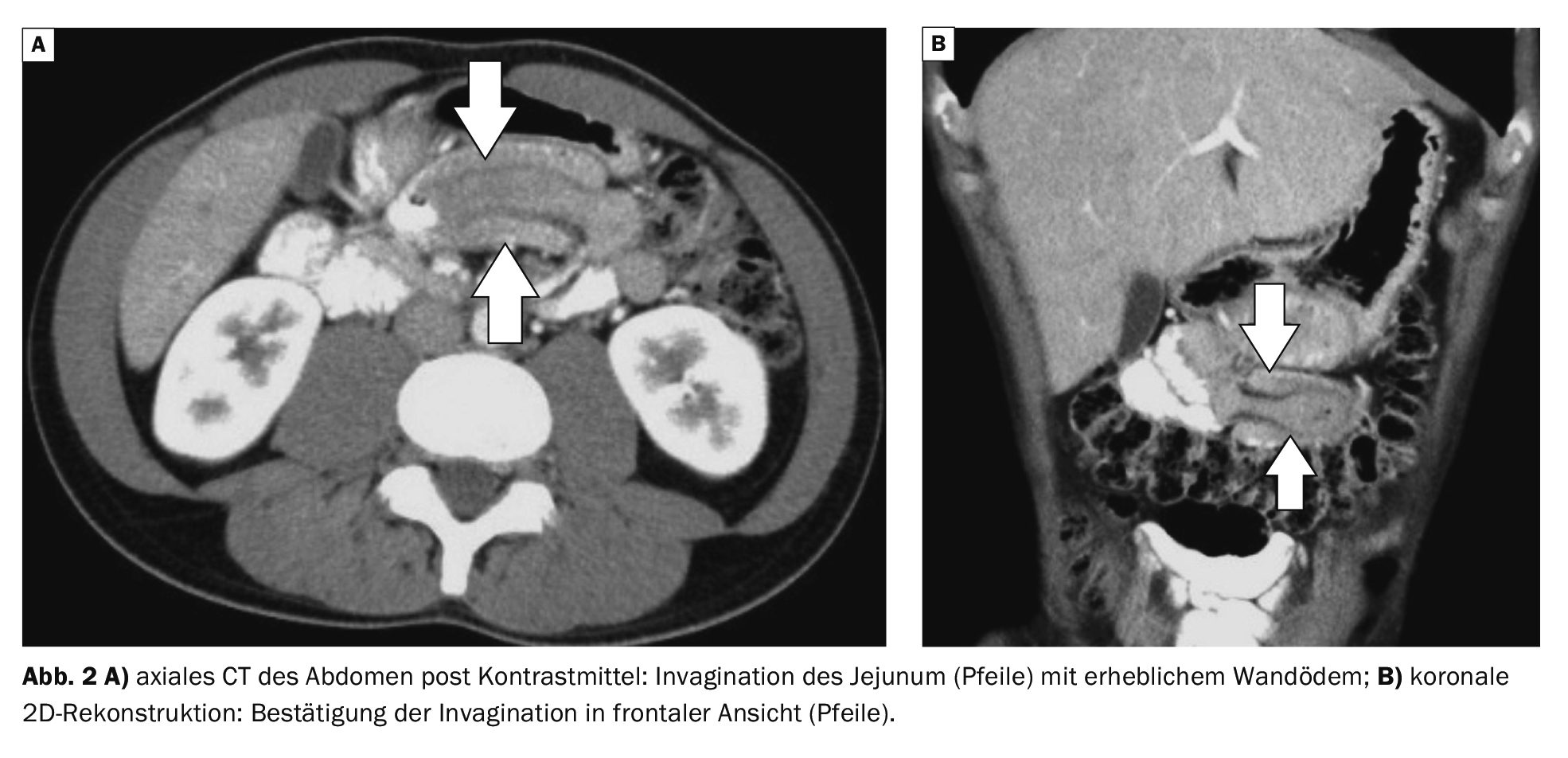
Computed tomographic diagnosis of intussusception should be considered primarily in adults or in children with a complicated course, particularly suspicious extrinsic compression [5]. Appropriate pediatric low-dose protocols have been developed for this purpose.
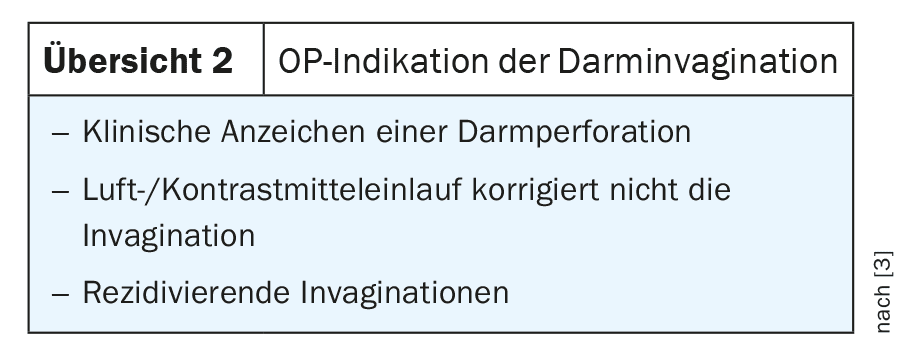
Magnetic resonance imaging examinations play a subordinate role in the diagnosis of intussusception. The method can be used to detect intestinal prolapse, also with regard to the assessment of neighboring body regions.
Case study
In case example 1 (Fig. 1A and B), an invagination of the terminal ileum into the cecum of about 1.2 cm is detectable in the MR-Sellink examination of a 56-year-old patient with known Crohn’s disease of the small bowel. The considerable wall edema of the small intestine led to stenosis of the lumen, thus widening the terminal ileum.
Case 2 demonstrates (Fig. 2A and B) the invagination of parts of the jejunum in an abdominal CT scan in a 28-year-old man with increasing pain symptoms in the middle abdomen.
Case 3 (Fig. 3A and B) shows the prolapse of the colonic segment into the anus-praeter pouch in an MRI scan of the abdomen in a 59-year-old patient during follow-up care for rectal cancer. There were no pain symptoms.
In case 4 (Fig. 4A and B), the displacement of the herniated small bowel loops to the right lateral side behind the lower edge of the liver can be seen. The patient had pain in the right middle and lower abdomen for about 4 weeks.
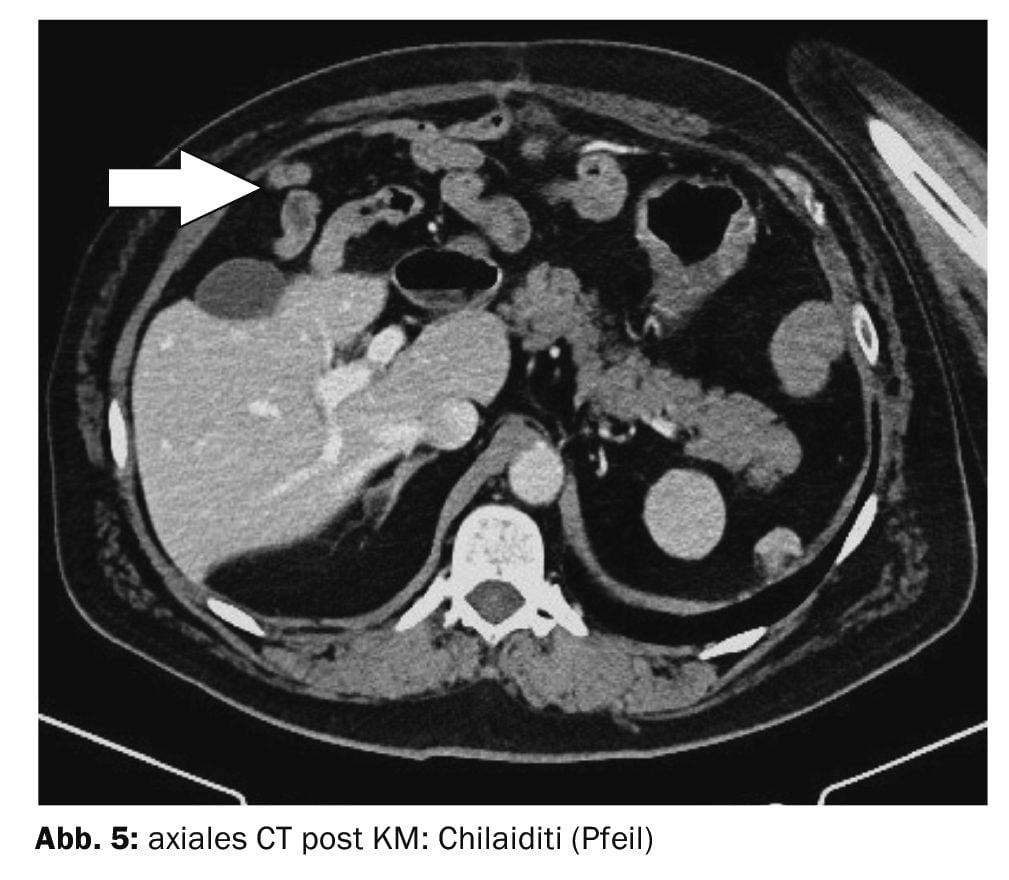
For comparison, case 5 shows a relatively harmless, in most cases asymptomatic displacement of the intestine between the liver and abdominal wall or diaphragm and liver: Chilaiditi syndrome (Fig. 5), named after the radiologist Dimitrios Chilaiditi [8]. The prevalence of the normal variant is 1%.
Take-Home-Messages
- Intestinal invagination is the invagination of a section of the intestine into the neighboring part of the intestine.
- The intussusception can occur in different parts of the intestine.
- Sudden stomach pain and intermittent, sometimes bilious vomiting, in many cases several times an hour, indicate the change.
- The diagnosis is made on the basis of clinical symptoms, palpation and imaging.
- The primary imaging procedure is sonography.
- If mechanical reduction is unsuccessful, there is a risk of intestinal wall ischemia with subsequent gangrene and acute peritonitis. Surgical treatment is then unavoidable at the latest.
Literature:
- “Anal and rectal prolapse”, www.amboss.com/de/wissen/anal-und-rektumprolaps,(last accessed 10/21/2024).
- “Chilaiditi syndrome”, https://flexikon.doccheck.com,(last accessed 21.10.2024).
- Cochran WJ: Intestinal intussusception, www.msdmanuals.com/de-de,(last accessed 10/21/2024).
- Hircin E, Haas I: Invagination, https://flexikon.doccheck.com/de/Invagination,(last accessed 21.10.2024).
- Prokop M, Galanski M (Eds): Spiral and Multislice Computed Tomography of the Body. Georg Thieme Verlag Stuttgart, New York 2003: pp. 586.
- Schrör S, Feichter M: Invagination: Symptoms, causes, therapy. www.netdoktor.de/krankheiten/invagination,(last accessed 21.10.2024).
- Staatz G, Schneider K: Differenzialdiagnose des akuten Abdomens. Part IV: Acute abdomen in children. Radiology up2date 2, 2010: 103-116.
- “Volvulus”, https://medlexi.de/Volvulus,(last accessed 10/21/2024).
FAMILY PHYSICIAN PRACTICE 2024; 19(11): 44-47