This case report concerns a 56-year-old woman with a long-standing diagnosis of Sjögren’s syndrome who was diagnosed with calcinosis cutis. After treatment of the calcinosis cutis, she was monitored for signs of CREST** syndrome – a special form of limited cutaneous systemic sclerosis.
In calcinosis cutis, insoluble calcium salts, mainly calcium hydroxyapatite or amorphous calcium phosphate, are deposited in the skin or subcutaneous tissue – most frequently in the area of the hands, in the periarticular tissue and over bony prominences. This results in hard, skin-colored or whitish papules and plaques that can break through the epidermis. The foci may be focal or scattered. They are solid deposits that vary in size from 1 millimeter to several centimeters. The clinical picture of calcinosis cutis varies: some patients present with asymptomatic nodules, while others experience pain, ulceration and infection. If the nodules are visible on the surface of the skin, this can be cosmetically disturbing. In addition to idiopathic forms, such calcifications form after skin injuries or as a result of connective tissue or metabolic diseases such as scleroderma and dermatomyositis. Like scleroderma and dermatomyositis, Sjögren’s syndrome is one of the collagenoses, but calcinosis cutis is comparatively rare. However, several case reports have been documented in the specialist literature [1–6]. Sjögren’s syndrome is an autoimmune disease that primarily attacks the salivary and lacrimal glands. A typical finding is dryness of the mouth, eyes and other mucous membranes (sicca syndrome) due to lymphocytic infiltration of the exocrine glands.
** Calcinosiscutis-Raynaudphenomenon-Esophagealdysmotility-Sclerodactyly-Teleangiectasia-syndrome
Dot-shaped white nodules in the area of the fingers
In a publication published in 2024, Akhila et al. reported on the case of a 56-year-old female patient who had been diagnosed with Sjögren’s syndrome 20 years ago [7]. At the time of diagnosis, oral and ocular sicca symptoms, strongly positive anti-Ro antibodies and a positive result in the Schirmer test were present. No biopsy findings of the salivary glands were documented in the available records. The patient’s disease course was characterized by asymptomatic elevation of creatinine kinase with negative myositis and muscular dystrophy panel, negative muscle biopsy results and chronic stable autoimmune thrombocytopenia. At the current time, her condition was well controlled with hydroxychloroquine (200 mg daily).
Current clinical picture: small yellowish-white nodules appeared on the fingertip of the right-sided digitus minimus. In the subcutaneous level there were painless, punctiform white nodules. There was no lymphadenopathy, telangiectasia, skin lesions, mucosal or skin ulcers. The joints were fully mobile, without redness, swelling or tenderness. The oral mucosa was dry. The rest of the physical examination findings were normal and all vital signs were within normal limits.
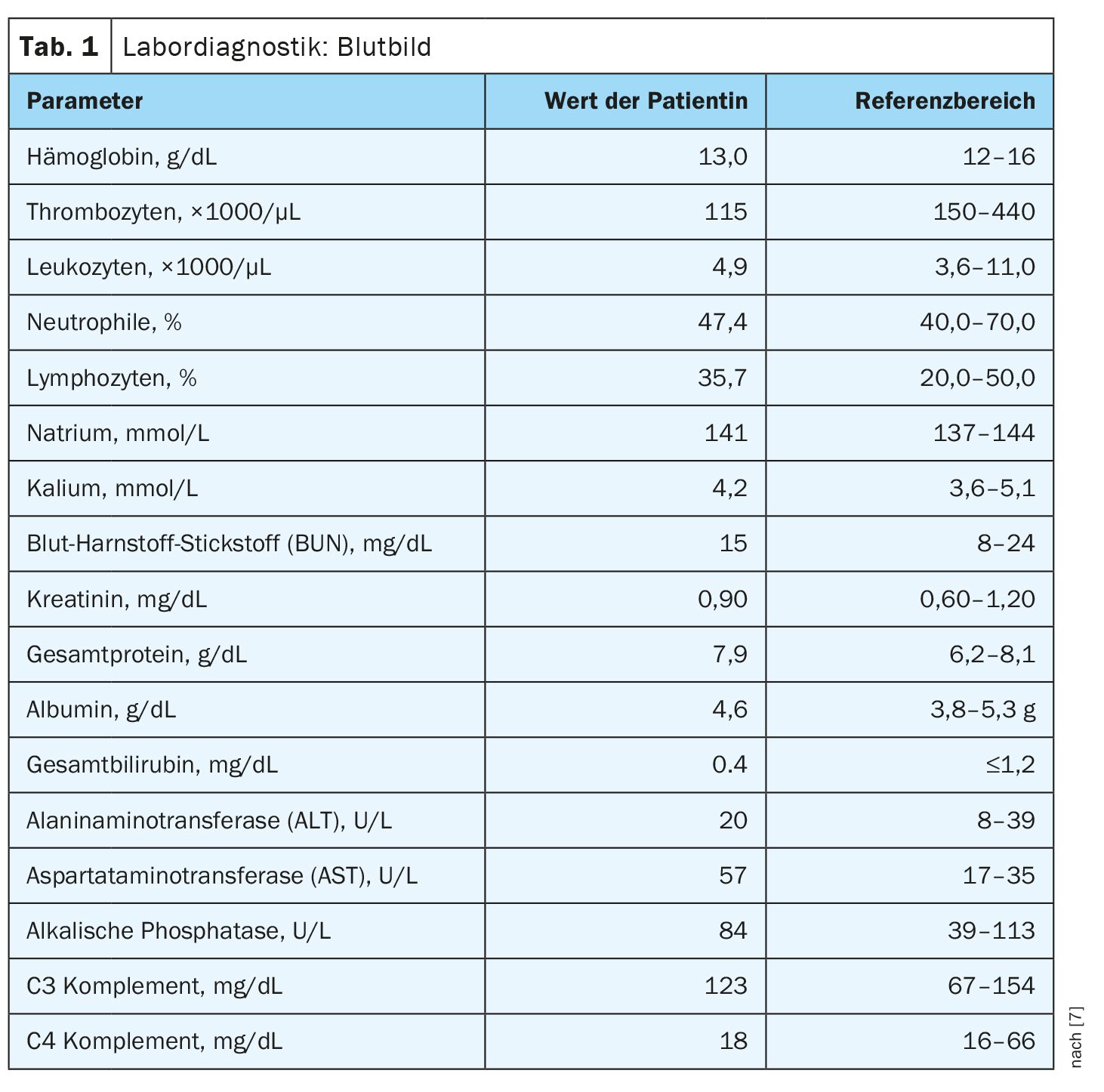
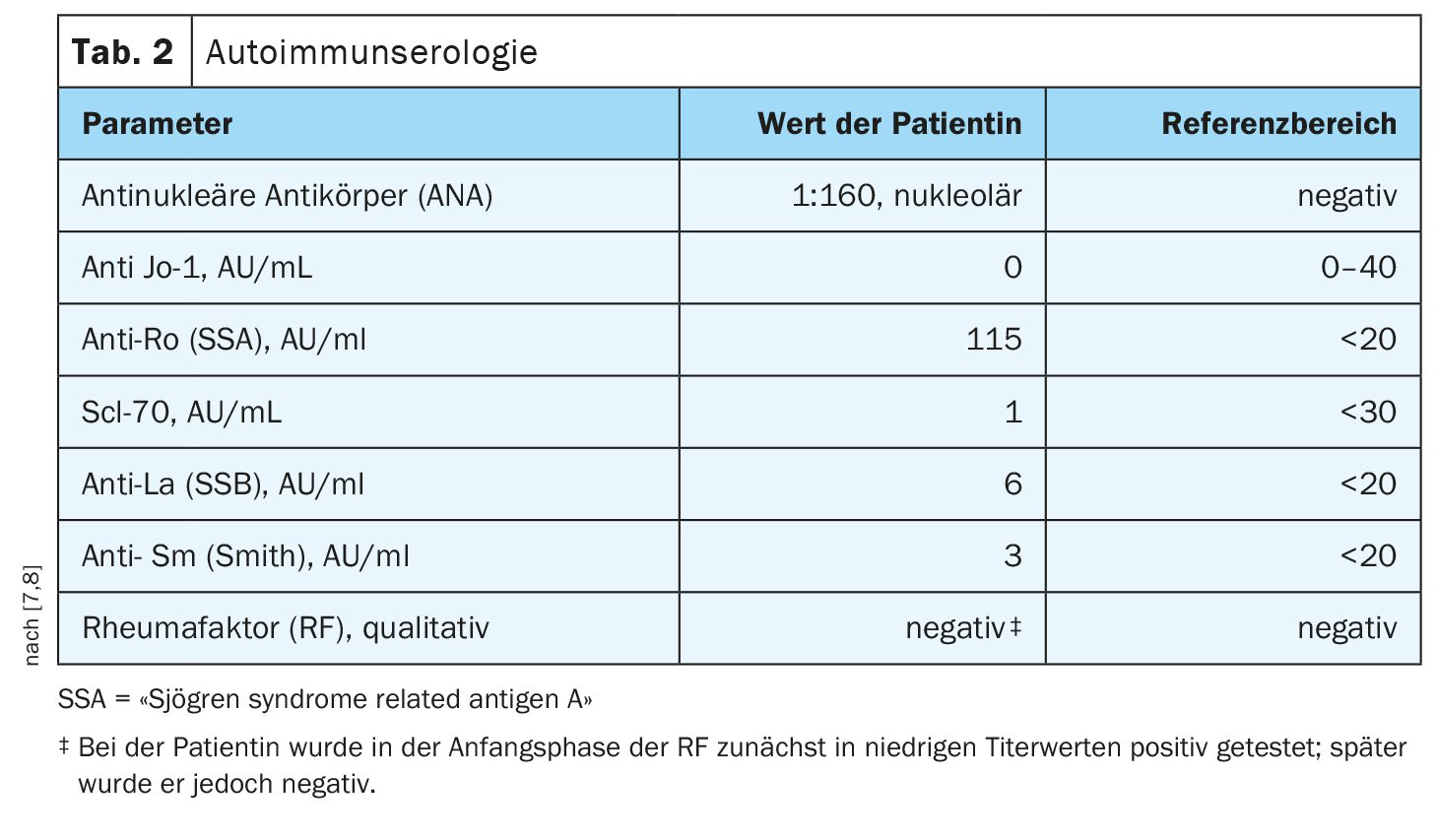
Diagnostics with autoimmune serology: The laboratory diagnostic parameters for renal function (Tab. 1) were within the normal range, as were the calcium and phosphorus levels. Autoimmune serology was positive for antinuclear antibodies with a titer of 1:160, nuclear pattern and anti-Ro (Sjögren’s syndrome type A) (Table 2). In addition, the X-ray of the right hand showed soft tissue calcifications in the distal first and fifth fingers. Previous skin biopsies showed no evidence of scleroderma, but biopsy findings of finger lesions on the right thumb and fourth finger were consistent with calcinosis.
Treatment and further course: As the symptoms in the finger area did not resolve with topical tretinoin (vitamin A derivative) and intradermal sodium thiosulfate injections, the patient was referred for surgical curettage of the calcinosis at her own request. Treatment of Sjögren’s syndrome was continued unchanged as disease activity was under control and inflammatory markers were normal. As calcinosis cutis is rare in Sjögren’s syndrome and the patient had a history of Raynaud’s phenomenon, she was monitored closely for other clinical or serologic signs of systemic sclerosis or CREST syndrome. CREST syndrome, also known as limited systemic sclerosis, is characterized by the combined presence of calcinosis cutis, Raynaud’s syndrome, esophageal motility disorders, sclerodactyly and telangiectasia. Affected patients develop skin tightening over the face and distally to the elbows and knees. A causal therapy for CREST syndrome is currently not available; treatment is symptom-related and interdisciplinary (dermatological, internal medicine and surgical).
Literature:
- Gonzalez-Ramos K, Ramsubeik K, Kaeley G: Case of calcinosis cutis associated with Sjogren’s syndrome. Clin Case Rep. 2023;11:e7628.
- Wasserman PL, et al: MR imaging findings of calcinosis cutis in primary Sjogren syndrome, a rare manifestation. Radiol Case Rep 2020; 15: 1029-1038.
- Yang CH, et al: Widespread dystrophic calcinosis cutis in both thighs associated with Sjögren’s syndrome: A case of 20-year follow-up. Kaohsiung J Med Sci 2019; 35: 648-650.
- Tsuchida Y, et al: Massive calcinosis cutis associated with primary Sjögren’s syndrome. BMJ Case Rep 2016; 2016:bcr2015214006.
- Fueki H, et al: Calcinosis cutis associated with primary Sjogren’s syndrome: strong expression of osteonectin and matrix Gla protein. Rheumatology (Oxford) 2011; 50: 2318-2320.
- Llamas-Velasco M, et al: Calcinosis cutis and Sjögren’s syndrome. Lupus 2010; 19: 762-764.
- Akhila APV, et al: A Case of Calcinosis Cutis in a Patient With Sjögren Syndrome: Annals of Internal Medicine: Clinical Cases 2024; 3; Number 6, www.acpjournals.org/doi/10.7326/aimcc.2023.1411,(last accessed 10.10.2024).
- MVZ Diamedis, www.diamedis.eu/humanmedizin/analysenverzeichnis.html?wp_page=detail&wp_code=1000000387,(last accessed 10.10.2024).
DERMATOLOGIE PRAXIS 2024; 34(5): 50–51