Case Report: In a 30-year-old female patient with lower extremity sensory disturbances, an MRI examination revealed multiple, vascular, tumor-like vertebral body lesions in the upper thoracic spine that corresponded to vertebral body hemangiomas.
Hemangiomas are venous malformations. At BWK 7, this showed extraosseous paravertebral and intraspinal extradural extension of the hemangioma. This caused narrowing of the spinal canal with compression of the myelon and centromedullary edema (Fig. 1a).
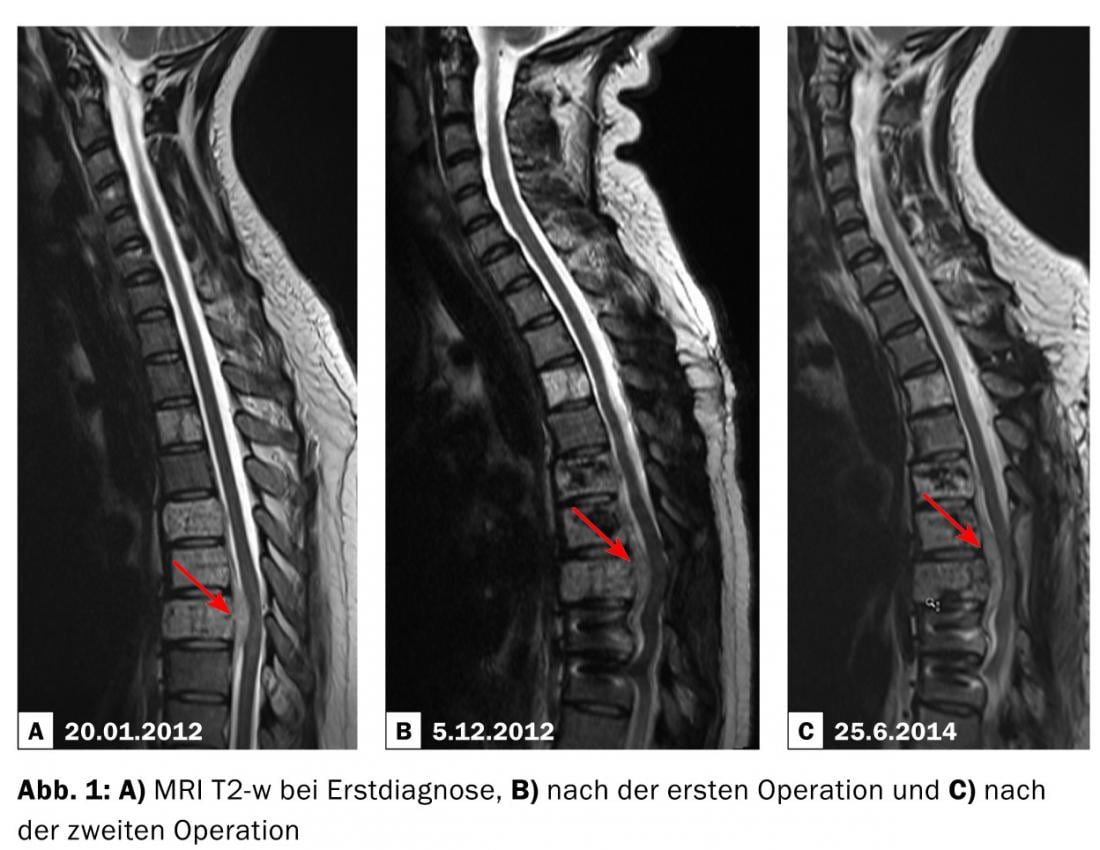
The patient underwent two surgeries at an out-of-town hospital, where dorsal decompression with stabilization via transpedicular screw fixation was performed (Fig. 1b) . Partial resection of the extraosseous hemangioma was not performed.
In the course, however, the symptoms worsened again with progressive neurological symptoms. In a follow-up MRI, a size progression of the intraspinal extradural hemangioma part was visible (Fig. 1c). This resulted in increasing myelon compression despite dorsal decompression.
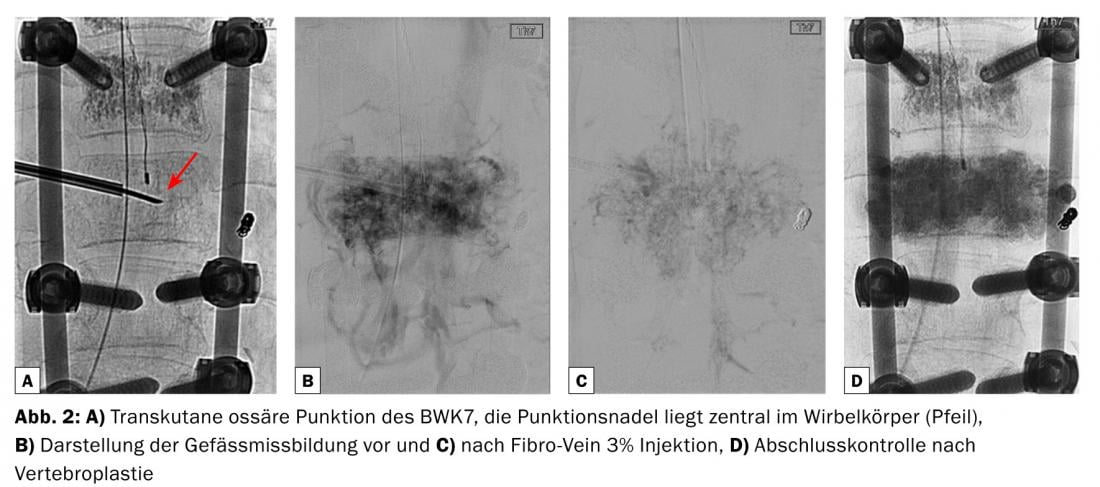
Interventional procedure: After an interdisciplinary discussion, it was decided to perform interventional therapy. Under intubation anesthesia, a transcutaneous puncture of BWK7 was performed (Fig. 2a) and after analysis of the vascular supply and especially the venous outflow of the intra- and paraosseous vascular malformation (Fig. 2b ), sclerotherapy was performed (Fig. 2c) . For this purpose, a sclerosing agent was injected (Fibro-Vein 3%), which leads to degeneration of the venous caverns via thrombosis. Vertebroplasty was performed at the same session, and bone graft substitute (DBX-DePuySynthes) was injected to stabilize the vertebral body (Fig. 2d). Periprocedurally, the patient received high-dose steroid therapy.
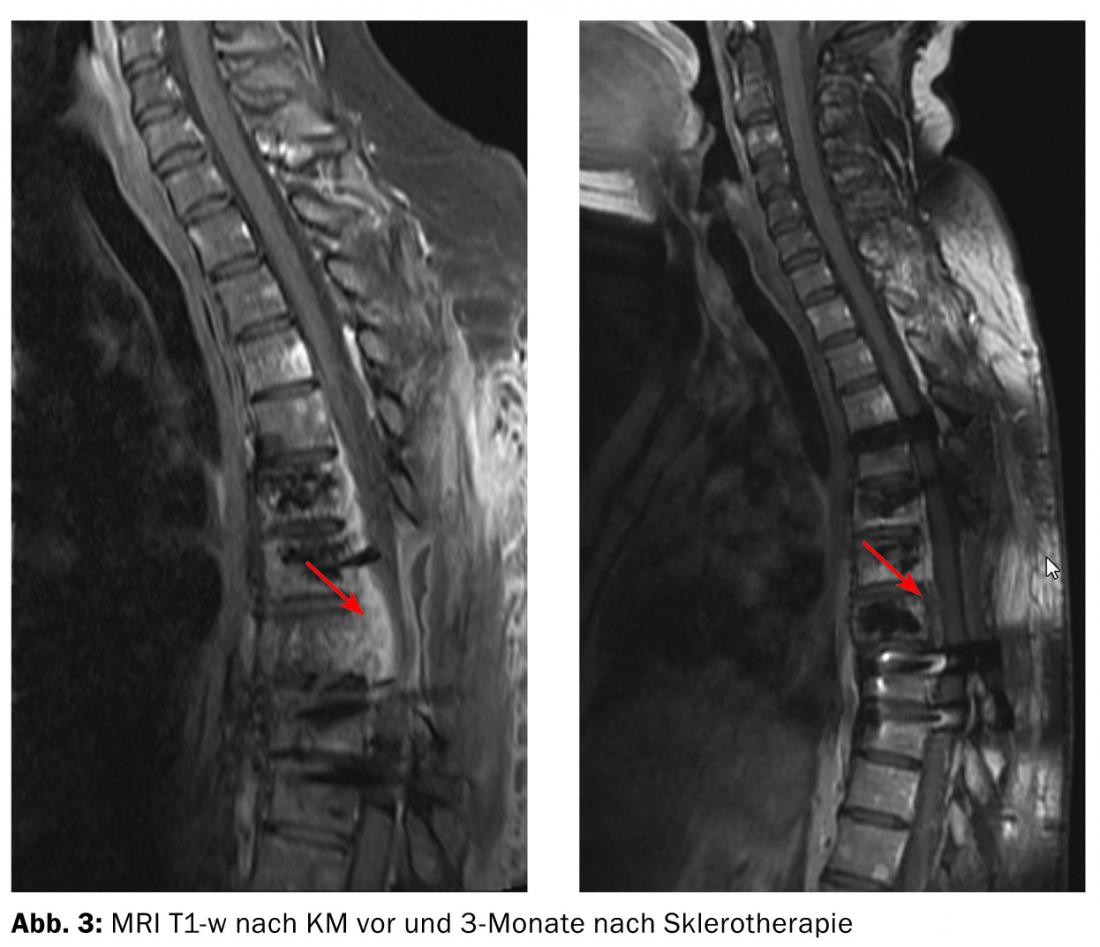
The 3-month follow-up showed a significant volume reduction of the intraspinal portion of the vascular malformation by more than 50% (Fig. 3). Myelon compression had completely regressed and a significant improvement in neurological symptoms had occurred.
SUMMARY ASSESSMENT: Vertebral hemangiomas are the most common benign avascular bone lesions of the spine often of dysembryogenetic or hamartous origin. They are usually incidental findings and do not require therapy. However, they may exhibit significant extraosseous aggressive growth and lead to neurologic symptoms, as in the previously described case. Minimally invasive interventional therapy of these venous vascular malformations represents an essential part in the treatment concept and should be considered in the therapy.
Kiriaki Kollia, MD
PD Dr. med. Zsolt Kulcsar
Prof. Dr. med. Isabel Wanke
Sophia L. Göricke, M.D.
InFo NEUROLOGY & PSYCHIATRY 2014; 12(6): 38-39.











