Malignant pleural mesothelioma is an aggressive tumor originating in the pleura. Patients have a short life expectancy after diagnosis, partly due to the limited treatment options. Exposure to asbestos fibers is considered the main risk factor for the development of pleural mesothelioma. As the disease progresses gradually over decades, it is often only discovered very late.
You can take the CME test on our learning platform after you have reviewed the recommended materials. Please click on the following button:
Malignant pleural mesothelioma is an aggressive tumor originating in the pleura. Patients have a short life expectancy after diagnosis, partly due to the limited treatment options. Exposure to asbestos fibers is considered the main risk factor for the development of pleural mesothelioma. As the disease progresses gradually over decades, it is often only discovered very late. For this reason, patients are often diagnosed with inoperable pleural mesothelioma, which is already at an advanced stage. This limits the therapeutic measures and is also reflected in a low life expectancy of around 12 months after diagnosis.
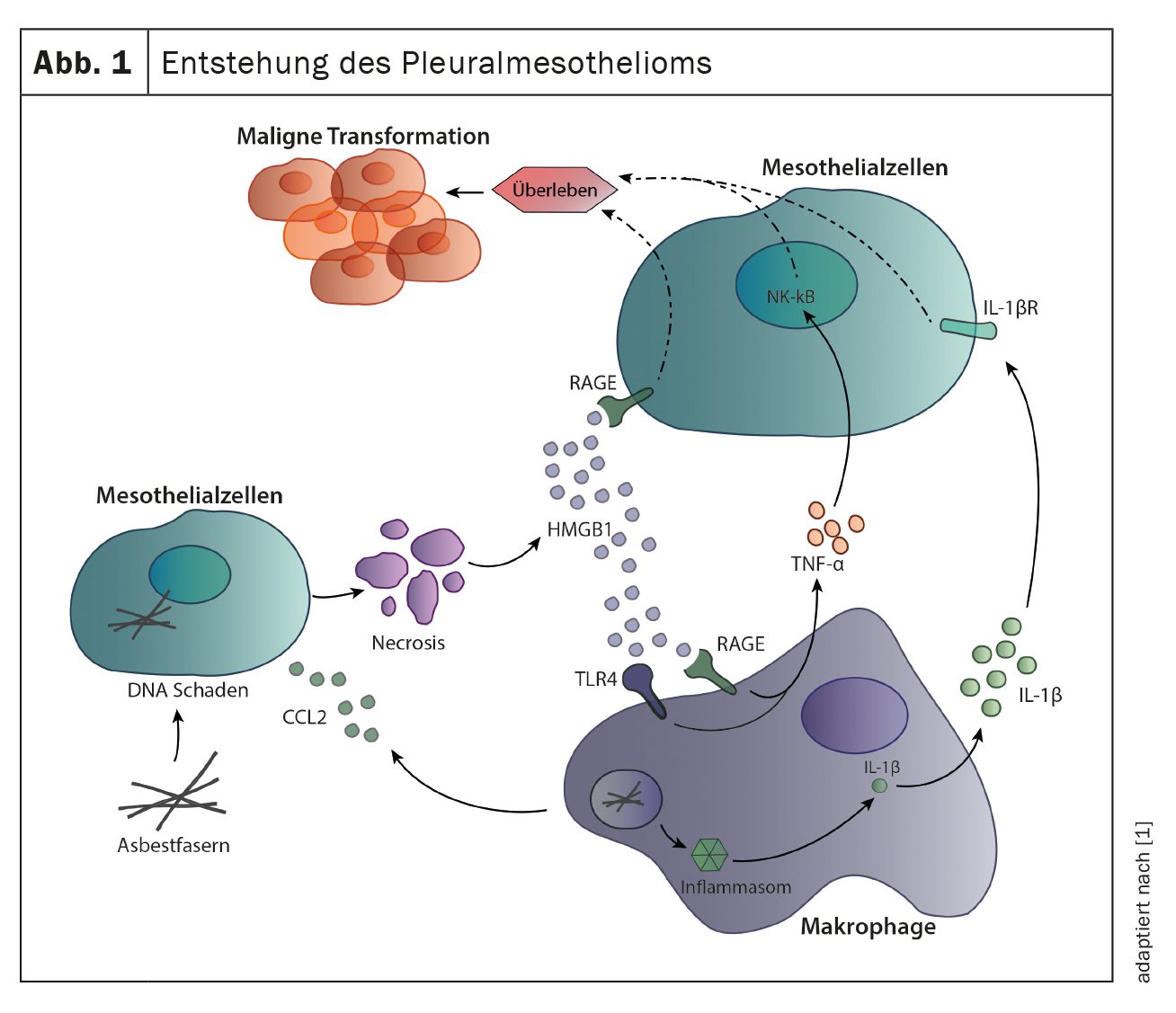
Development of pleural mesothelioma
The most common cause for the development of pleural mesothelioma is exposure to asbestos fibers, usually decades before the onset of symptoms. Inhalation of the fibers leads to chronic inflammation of the pleura, which contributes to malignant transformation of mesothelial cells. The fibers can directly cause DNA damage in mesothelial cells, leading to cell death and the release of inflammatory mediators such as HMGB1 and CCL2. Inflammatory mediators, especially CCL2, recruit macrophages and act directly on mesothelial cells by binding to RAGE receptors on mesothelial cells and inducing their cell division and migration. Recruited macrophages also contribute to local inflammation and proliferation of mesothelial cells. The uptake of asbestos fibers by macrophages stimulates the immune sensor inflammasome, which leads to the secretion of IL-1β. In addition to IL-1β, macrophages also secrete TNF-α, both cytokines contribute to the survival of mesothelial cells and their further malignant transformation (Fig. 1) [1].
Gene signatures
Approximately 80% of tumors are caused by exposure to asbestos decades earlier. A familial genetic predisposition due to germline mutations in the BAP1 genecan increase the likelihood of developing pleural mesothelioma. In contrast to other tumour diseases, in which activating mutations in oncogenes are frequently present, pleural mesothelioma is primarily characterized by the alteration and loss of entire chromosome parts and by mutations in tumour suppressor genes. For a long time, little attention was paid to genetic alterations in pleural mesothelioma due to the low mutation rate of this type of cancer and a few cases where targeted therapy would be possible. The most common mutations and deletions affect the genes BAP1, CDKN2A and NF2. BAP1 is a tumor suppressor gene involved in DNA damage repair and cell cycle control. BAP1 is altered in approximately 45% of all pleural mesotheliomas, although this figure may vary between different histologies.
CDKN2A is also a tumor suppressor gene that is frequently deleted in pleural mesothelioma. Changes in this gene are found in approximately 47% of all tumors. CDKN2A plays an important role in the regulation of the cell cycle, it codes for the inhibitor of cyclin-dependent kinase 4 and 6. Loss of this gene therefore leads to pro-mitotic signals and cell survival.
NF2 is also involved in cell cycle regulation and is altered in approximately 32% of all pleural mesotheliomas. NF2 regulates the Hippo signaling pathway via the proteins YAP and TAZ. Inactivation of NF2 leads to hyperactivated YAP and uncontrolled cell division.
Only a few pleural mesotheliomas have mutations in genes that can be specifically treated with small molecule inhibitors. We were able to show in a study that the genes ALK, KRAS EGFR, PDGFRA/B, ERBB2 or FGFR3 are mutated in about 5% of all pleural mesotheliomas, which could be treated with targeted therapies [2]. Further studies have yet to demonstrate the effectiveness of this treatment in pleural mesothelioma.
Tumor environment
The interaction of different cell types such as immune cells, stromal cells, tumor cells and endothelial cells of the blood vessels in the tumor is very complex and has not yet been fully researched in pleural mesothelioma. Depending on the tumor type and patient, the heterogeneity of cell types and functions is great. This makes it difficult to develop therapies that act directly on the tumor environment. In addition, the immune cells often have an inhibitory and regulatory phenotype, mainly represented by regulatory T cells, type 2 macrophages and myeloid suppressor cells.
Macrophages are the most common immune cells in pleural mesothelioma and are recruited from the blood by CCL2 secreted by mesothelial cells in the form of monocytes. Tumor-associated macrophages express an immunosuppressive type 2 phenotype and support the proliferation of malignant mesothelial cells and tumor growth, which also correlates with a poor prognosis. The second most common immune cells in pleural mesothelioma are T lymphocytes, with all subtypes such as CD4+ T helper cells, CD8+ cytotoxic T cells and FoxP3+ regulatory T cells present. Cytotoxic T cells often express markers such as Lag-3, Tim-3, PD-1, which define a non-reactive phenotype. These T cells are no longer able to perform effector functions, which gives the tumor cells a survival advantage. The presence of T cells in the tumor is positively associated with survival in pleural mesothelioma, depending on the study, but this may vary depending on the histology and the specific phenotypes of the T cells. For example, regulatory T cells in the tumor are associated with shorter survival. Other suppressive immune cells in the tumor are myeloid suppressor cells, which can account for up to 10% of all infiltrating immune cells. They have a negative effect on T cells and can inhibit their cell division.
Pathology
Pleural mesothelioma is divided into three histological subtypes: epithelioid (approx. 80% of cases), biphasic and sarcomatoid pleural mesothelioma. The biphasic subtype is characterized by a combination of epithelioid and sarcomatoid structures.
The histological subtypes differ primarily in terms of life expectancy. Patients with an epithelioid pleural mesothelioma have a longer life expectancy compared to patients with a biphasic or sarcomatoid pleural mesothelioma. In addition, patients with an epithelioid subtype usually benefit from resection, whereas the other subtypes do not benefit from surgery. Sometimes the diagnosis of pleural mesothelioma is difficult due to the cellular morphology, as the pleura is often altered by inflammatory changes or metastases of another malignant disease are present. For this reason, further analysis of a pleural biopsy using immunohistochemistry (IHC) of two mesothelioma markers such as calretinin, podoplanin, Wilms’ tumor-1 (WT-1) or cytokeratin 5/6 is necessary. In addition, other carcinomas can be excluded by staining with CEA, Ber-EP4, pancytokeratin or claudin-4. A pleural mesothelioma with a squamous cell-like change can be differentiated from a squamous cell carcinoma by staining for the markers p40 and p63. Furthermore, genetic alterations in the BAP1 and CDKN2A genes often occur, resulting in a loss of expression of these proteins in the tumor. For this reason, immunohistochemical analysis of BAP1 and MTAP expression (MTAP is analyzed as a proxy for CDKN2A, as these genes are located directly next to each other on chromosome section 9p21 and there is often a co-deletion) can also be helpful for the final diagnosis.
Symptoms, diagnosis and staging
Patients often present with vague symptoms of dyspnea, chest pain and weight loss. Patients often present with a unilateral pleural effusion. The diagnosis of pleural mesothelioma is made by several examinations: i) radiologic examinations including CT of the thorax, ii) pleural biopsy by thoracoscopy for further verification of the diagnosis of pleural mesothelioma and determination of the histology. A pleural biopsy should therefore always extend into the subpleural fat and be performed from three or more different locations. To avoid the risk of implantation of tumor cells in the chest wall, only 1-2 thoracoscopic entry points should be used [3]. Preferably, these should be placed in the same intercostal space as the macroscopically complete resection planned later.
Staging is performed using positron emission tomography (PET-CT) and is supplemented by mediastinoscopy or endobronchial ultrasound (EBUS) in the case of suspected involvement of the mediastinal lymph nodes, by contralateral thoracoscopy in the case of suspected involvement of the contralateral pleura, or by laparoscopy in the case of suspected involvement of the peritoneum. Magnetic resonance imaging (MRI) of the thorax can also provide valuable staging information about infiltration of the diaphragm, chest wall, pericardium or mediastinum.
Surgical interventions
The treatment should be discussed in an interdisciplinary Tubmorboard with specialists from thoracic surgery, oncology, radiation oncology, pathology and radiology. If the patient qualifies for a multimodal treatment concept in terms of tumor stage and general condition, re-staging using PET-CT is performed after neoadjuvant chemotherapy with platinum-containing cytostatics and folic acid antagonists to reassess operability. Due to the anatomical situation with proximity to mediastinal structures, sufficient safety margins cannot be maintained during MPM resection. A radical resection therefore means a macroscopically complete resection with the aim of maximum cytoreduction, but with the risk of a residual microscopic tumor [4]. A macroscopically complete resection can be achieved by means of an extrapleural pneumonectomy (EPP) or a lung parenchyma-preserving extended pleurectomy and decortication (EPD) [4]. While EPP involves en bloc resection of the affected lung with visceral and parietal pleura, diaphragm and pericardium, EPD involves detaching only the parietal and visceral pleura and removing it together with the affected diaphragm and pericardium, leaving the lung intact [4]. If there are no signs of pericardial or diaphragmatic involvement, an isolated pleurectomy and decortication (PD) can be chosen. In all surgical resections, a systematic mediastinal lymphadenectomy should also be performed. In recent years, there has been an increasing shift from EPP to EPD, as the lung parechyma and functional reserves are preserved, thus allowing the patient a better quality of life. Furthermore, EPP is also associated with increased perioperative morbidity and mortality. EPP should only be considered in selected cases with extensive infiltration of the lung parenchyma and sufficient cardiopulmonary reserves and should only be performed at experienced centers.
In patients in whom maximum cytoreduction by means of macroscopic complete resection is not an option, the recurrence of a symptomatic pleural effusion can be prevented in a palliative approach. In the case of extensive lungs, this is done by means of thoracoscopic talc pleurodesis, in the case of chronically trapped lungs by means of a subcutaneously tunneled catheter system, which can also be used for regular effusion drainage in the home environment.
Palliative VATS-PP is recommended to control recurrent pleural effusions in patients who are fit enough for surgical treatment and cannot benefit from chemical pleurodesis (or after an unsuccessful pleurodesis) or an indwelling catheter [5].
System therapy
Since 2004, patients have been treated with a systemic combination therapy of pemetrexed and platinum-based chemotherapy. The introduction of bevacizumab, an angiogenesis inhibitor, in combination with cisplatin/pemetrexed has increased life expectancy by approximately 2.5 months. Based on the success of immune checkpoint inhibitors in various solid tumors, the combination therapy of ipilimumab (anti-CTLA-4 antibody) and nivolumab (anti-PD-1 antibody) was tested. This therapy showed a significant improvement in survival in sarcomatoid pleural mesothelioma and epithelioid with PD-L1>1% [6]. As a result, this treatment was approved by the FDA and EMA as first-line therapy in 2020. However, in later lines of treatment, pleural mesothelioma still remains a disease without standardized treatment methods and patients are often enrolled in clinical trials.
Take-Home-Messages
- In selected patients with early-stage MPM and sufficient cardiopulmonary reserves, maximum surgical cytoreduction by means of macroscopic complete resection is recommended.
- A macroscopically complete resection should always be performed as part of a multimodal treatment concept in combination with chemotherapy.
- Treatment recommendations and decisions should always be made at an interdisciplinary thoracic oncology tumor board in the presence of oncologists, radiation oncologists, pulmonologists and thoracic surgeons.
- First-line therapy in non-operable patients is based on nivolumab and ipilimumab for patients with epitelioid pleural mesothelioma with PD-L1 expression >1% and for all other histologic subtypes. Otherwise, treatment with platinum-pemetrexed and bevacizumab is the other option.
Literature:
- Hiltbrunner S, Mannarino L, Kirschner MB, et al.: Tumor Immune Microenvironment and Genetic Alterations in Mesothelioma, Frontiers in oncology 11 (2021) 660039.
- Hiltbrunner S, Fleischmann Z, Sokol E, Curioni-Fontecedro A: 1734P Genomic landscape of pleural and peritoneal mesothelioma tumors, Annals of Oncology 32 (2021) S1200.
- Kindler HL, Ismaila N, Armato SG, et al.: Treatment of Malignant Pleural Mesothelioma: American Society of Clinical Oncology Clinical Practice Guideline, J Clin Oncol 36(13) (2018): 1343–1373.
- Rice D, Rusch V, Pass H, et al.: Recommendations for uniform definitions of surgical techniques for malignant pleural mesothelioma: a consensus report of the international association for the study of lung cancer international staging committee and the international mesothelioma interest group, J Thorac Oncol 6(8) (2011): 1304–1312.
- Opitz I, Scherpereel A, Berghmans T, et al.: ERS/ESTS/EACTS/ESTRO guidelines for the management of malignant pleural mesothelioma, Eur J Cardiothorac Surg 58(1) (2020): 1–24.
- Baas P, Scherpereel A, Nowak AK, et al: First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomized, open-label, phase 3 trial, Lancet 397(10272) (2021) 375-386.
InFo ONKOLOGIE & HÄMATOLOGIE 2024; 12(6): 6–9