Depression is one of the most common diseases worldwide. In addition to the classic pharmacological therapy methods, lifestyle methods are increasingly becoming the focus of the therapeutic armamentarium. Exercise and the treatment of insomnia show a beneficial effect, whereas the role of diet has not yet been conclusively established.
Depression is one of the most common diseases worldwide. According to the projections of the World Health Organization (WHO), it will be in first place in 2030 [1]. According to the currently valid diagnostic system, the disease is divided into the severity levels mild, moderate and severe, with the more severe disease requiring the most intensive – in some cases also inpatient – therapy. In accordance with the biopsychosocial approach, various evidence-based psychotherapeutic and pharmacotherapeutic procedures are available for this purpose, which are usually applied in a multimodal approach. Although this broad therapeutic approach can help many patients and achieve remission, up to 30% have an inadequate response to treatment. In this context, the question arises whether, in addition to the classical procedures, newer approaches derived from the so-called lifestyle procedures can contribute to improving the therapeutic armamentarium. In the following, therefore, the aspects of nutrition, sport and sleep will be examined.
Depression and nutrition
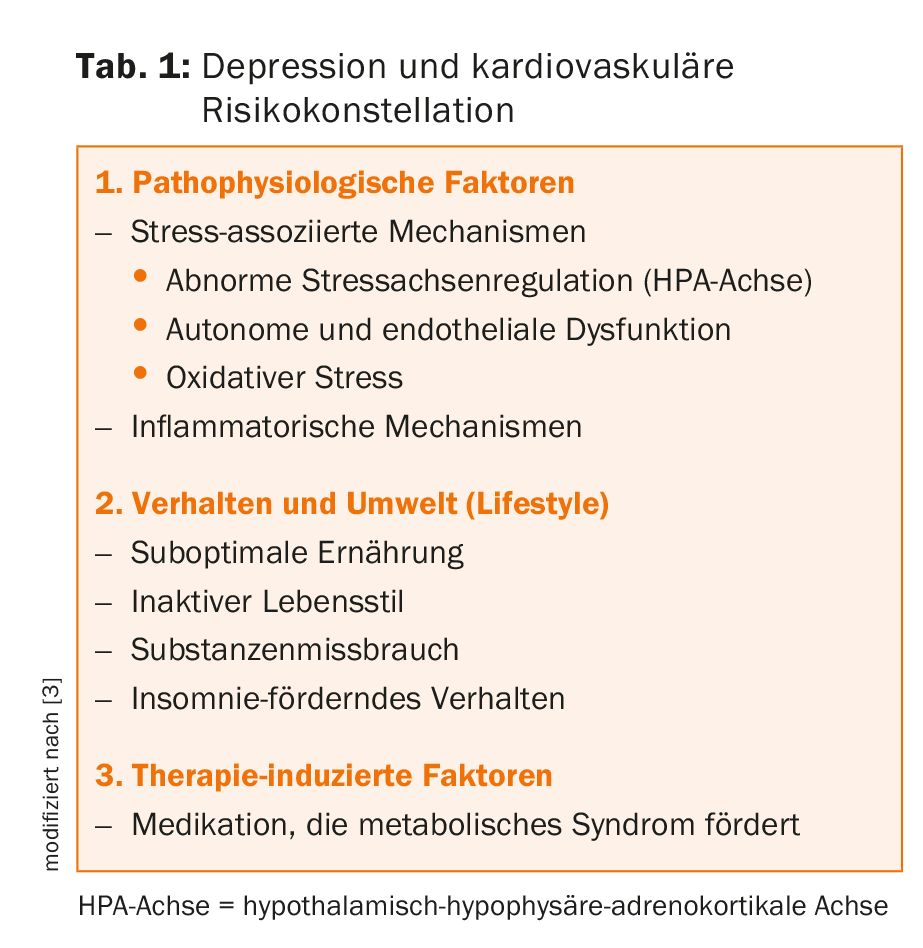
Patients with depression as a stress-associated condition have higher morbidity and a significantly increased risk of metabolic syndrome compared with healthy individuals [2]. In addition, many prospective studies show that the presence of depression adversely affects the outcome of cardiovascular disease [3] (Table 1) .
There are some hypotheses about the reasons for the above observations:
- Pathophysiological changes caused by depression: Overactive stress axis activity (hypothalamic-pituitary-adrenocortical axis, HPA axis), autonomic dysfunction associated with oxidative stress and endothelial dysfunction, or alterations in inflammatory regulatory circuits are likely to be important factors.
- The behavioral changes caused by depression, such as inactivity, unfavorable diet, and addictive substance use (tobacco and alcohol), reinforce these unfavorable factors.
- Psychopharmacologic medication may promote metabolic syndrome. Therefore, care should be taken in psychopharmacological therapies to use medications that are as weight-neutral as possible.
Contrary to the finding that the aforementioned changes in the context of depression are risk factors for cardiovascular disease, conversely, some studies indicated that a Mediterranean diet high in vegetables, fruits, fish, and unsaturated fatty acids (olive oil) but low in red meat and saturated fats may contribute to a reduced risk of depression [4]. The extent to which this association can be explained pathophysiologically is unclear. Recent findings suggest that, at most, the gut microbiome may be a mediator and have an impact on the development of psychological symptoms such as anxiety and depression [5]. Current research addresses the question of which mechanisms play a role here, and could contribute to depression development such as inflammatory or stress axis regulation [6]. It remains to be seen whether this will lead to therapeutic approaches that go beyond dietary recommendations.
Depression and sport
In contrast to diet, recommendations on physical activity have already found their way into treatment recommendations [7]. The interest in including sport or controlled physical activity in the standardized treatment repertoire for depression is based on the following factors: the findings on morbidity and metabolic risks arising from depression, depression-related behavioral changes (inactivity and lack of motivation), and the need for additional treatment options in view of the poor drug therapy response of a maximum of 30% [8].
Initial controlled studies demonstrated that a sports endurance program may have a dose-dependent antidepressant effect [9]. The majority of the studies conducted below on the effectiveness of exercise interventions are based on studies with outpatients and mild to moderate depressive symptomatology. They showed different effect sizes, but with a clear preponderance in favor of sports interventions compared to the placebo group, group without treatment and group with standardized regular treatment of depressed patients [10]. Subanalysis of studies with a placebo intervention and high methodological standards found significantly smaller effect sizes, but they still remained clinically significant [11]. Currently, according to the study protocols, the minimum recommended dose is an exercise program of ≥45 minutes three times per week in the aerobic pulse range (50-80% of maximum pulse) for 10-12 weeks, with an additional targeted motivational support program to be implemented in more severe disease. A positive effect could already be shown after four weeks [12]. With regard to the above-mentioned links between depression and diet, it was also shown that training for several weeks could positively influence the metabolic syndrome in hospitalized depressive patients [13].
Cognitive impairment in depression
A distinctive feature of depression is cognitive decline, which, although potentially reversible, appears difficult to treat with standard psychotherapeutic or pharmacotherapeutic interventions [14]. In particular, these include impairments in attention, executive functions, and memory [15].
Since (1.) in healthy individuals, imaging techniques have shown that people without regular physical training have to activate more brain regions to achieve the same cognitive performance as physically trained individuals, and (2.) protective effects of regular physical activity on cognitive functions have already been demonstrated in dementia, it is obvious to investigate physical activity in depressives, especially for its cognitive effects [16]. Initial studies demonstrated that in moderately depressed patients with subjective cognitive impairment, endurance training over a standardized treatment period of twelve weeks was able to significantly improve cognitive functions [17]. Our own studies in moderately to severely depressed, hospitalized and multimodal treated patients could demonstrate an improvement of attention as well as working memory by an additional endurance training over six weeks [18]. Further studies should replicate these results and hopefully lead to a better evidence-based foundation for treatment recommendations of exercise in depressed patients with cognitive dysfunction.
Psychological, neurobiological and immunological mechanisms.
Improved body awareness, an increase in self-confidence and self-efficacy accompanied by improved affect regulation are considered to be psychological impact factors of sport. In addition, various improvements of neurobiological mechanisms on the effects of sport on depression are discussed (Tab. 2). Thus, the influence on neuroendocrine regulation, i.e. HPA-axis regulation, has been well documented for several decades [19]. In healthy individuals, regular exercise has been shown to influence the HPA axis: Thus, marathon runners showed a phase advance in the HPA axis with earlier morning increase of cortisol, whereas the 24-h rhythm showed no difference compared to the group without training [20]. Although a relative increase in cortisol is seen in high performance athletes, cortisol appears to be converted to the inactive cortisone more rapidly in trained individuals than in untrained individuals, which is thought to have a protective effect with respect to the development of depressive episodes [21]. Initial, smaller studies using HPA axis function tests such as cortisol awakening response (CAR), which are more informative than simple plasma level determinations, also demonstrated a beneficial effect on HPA axis regulation in depressed patients [22].
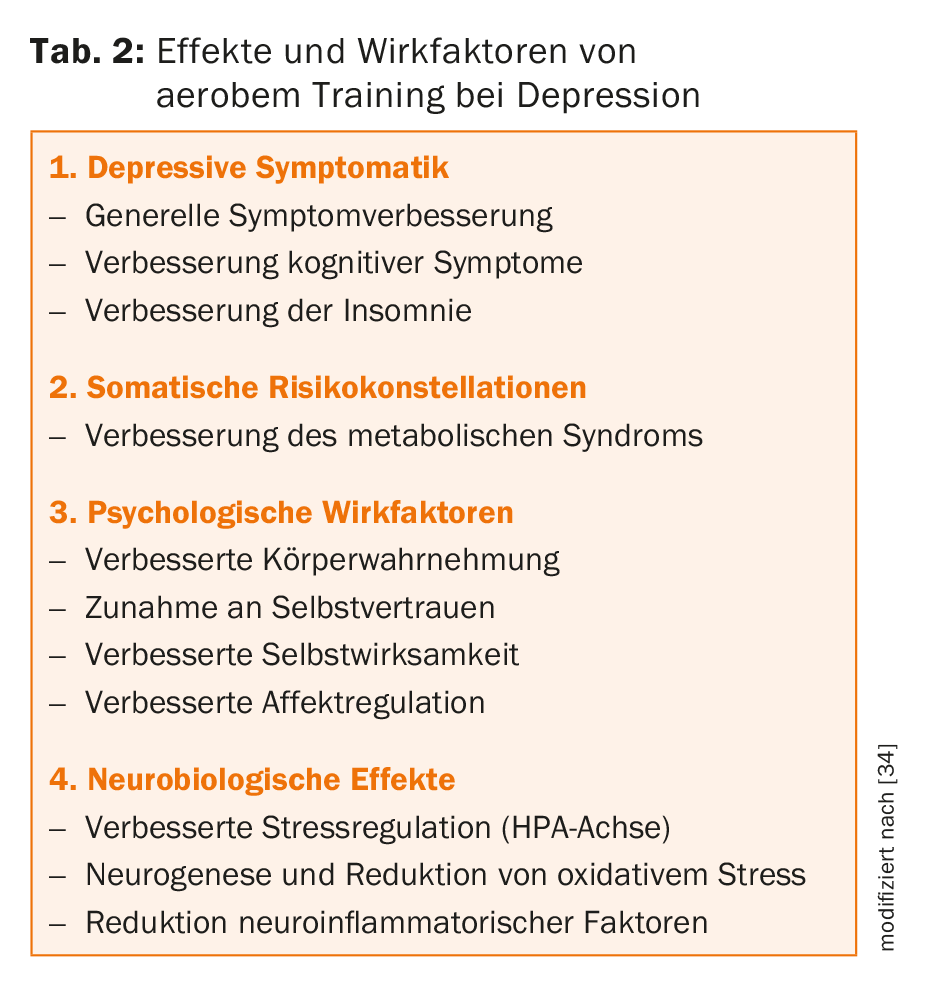
Another mechanism associated with depression is neurogenesis, reflected by brain-derived neurotrophic factor (BDNF) as a clinically measurable biomarker [23]. Preclinical models have shown that hippocampal neurogenesis can be activated by regular physical activity [24]. It is likely that these effects are mediated in part via BDNF, but clear evidence in humans is still lacking [25].
Some studies also suggest that exercise may also reduce neurotoxic substances and thus oxidative stress in depression [26,27]. Finally, recent hypotheses postulate that immunological mechanisms are also thought to be linked to depression and that sports interventions could favorably influence them [28]. For example, TNFα was recently identified as a pro-inflammatory cytokine that was predictive of therapeutic response to exercise intervention in depressed individuals [29].
Depression and sleep
Insomnia complaints are among the leading symptoms in depression. Sleep changes can be visualized on polysomnography and characteristically include a reduction in deep sleep and characteristic changes in rapid eye movement (REM) sleep with advancement to the first half of the night and an increased number of eye movements in REM sleep (so-called REM density) in moderately to severely depressed patients. With successful treatment of depression, these sleep changes remit; however, if they persist, they are a predictor of recurrence of a depressive episode [30]. Insomnia is thus not only a symptom but also a predictor of the onset of depression [31]. Maintaining a regular day-night rhythm is therefore an important component in both the prophylaxis and treatment of depression. If sleep disorders persist in depressed patients, they should be treated intensively in the sense of relapse prophylaxis. In addition to psychotherapeutic and pharmacotherapeutic measures, sport can also be helpful here. Thus, not only did patients with primary insomnia benefit from several weeks of controlled aerobic training [32], but also patients with depression-associated insomnia showed significant improvement with a twelve-week endurance program [33].
Summary
In summary, in addition to psycho- and pharmacotherapeutic treatment approaches for depression, lifestyle elements are increasingly being incorporated into a multimodal therapeutic approach. Thus, many studies suggest that exercise can be helpful as an additional intervention for depressed patients – and not only for mild – but also for moderate and severe depression. In particular, cognitive symptoms, which are otherwise difficult to influence, could be a specific target for such a therapeutic program. In addition, cardiovascular risks associated with depression are also favorably influenced. The extent to which interventions targeting dietary habits (Mediterranean diet) or manipulation of the intestinal microbiome have a place in depression treatment cannot be assessed at this time. On the other hand, the targeted treatment of insomnia complaints should have a permanent place, as this has also been shown to improve the long-term prognosis of depression in cases of stable remission. Maintaining a stable day-night rhythm is just as much a part of this as dealing constructively with stress.
Take-Home Messages
- Cognitive symptoms of depression are difficult to treat and have a large impact on social functioning (work!).
- Exercise can be helpful as an adjunctive treatment and has particularly positive effects on depressive-cognitive symptoms.
- Nutritional factors and the intestinal microbiome may be factors in depression genesis.
- Insomnia is a risk factor for depression as well as a symptom of depression. Their successful treatment reduces the risk of recurrence of depression.
Literature:
- Murray CJL, et al. : Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of disease study 2010. Lancet 2012; 380: 2197-2223.
- Chandola T, Brunner E, Marmot M: Chronic stress at work and the metabolic syndrome: a prospective study. BMC 2006; 332(7540): 521-525.
- Goldstein BI, et al: Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: A scientific statement from the American heart association. Circulation 2015; 132(10): 965-986.
- Psaltopoulou T, et al: Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann Neurol 2013; 74(4): 580-591.
- Foster JA, McVey Neufeld KA: Gut-brain axis: how the microbiome influences anxiety and depression. Trends in Neuroscinces 2013; 36: 305-312.
- Sarkar A, et al: Psychobiotics and the manipulation of bacteria-gut-brain signals. Trends in Neurosciences 2016; 39: 763-781.
- DGPPN: S3-Leitlinie – Unipolare Depression, Langfassung. 2nd edition, version 5, AWMF register no.: nvl-005. 2015.
- Warden D, et al: The STAR*D Project results: a comprehensive review of findings. Curr Psychiatry Rep 2007; 9(6): 449-459.
- Dunn AL, et al: Exercise treatment for depression: efficacy and dose response. Am J Prev Med 2005; 28(1): 1-8.
- Josefsson T, Lindwall M, Archer T: Physical exercise intervention in depressive disorders: a meta-analysis and systematic review. Scand J Med Sci Sports 2014; 24(2): 259-272.
- Kvam S, et al: Exercise as a treatment of depression: A meta-analysis. J Affect Disord 2016; 202: 67-82.
- Rethorst CD, Trivedi MH: Evidence-based recommendations for the prescription of exercise for major depressive disorder. J Psychiatr Pract 2013; 19(3): 204-212.
- Kerling A, et al: Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord 2015; 177: 1-6.
- Papakostas GI: Cognitive symptoms in patients with major depressive disorder and their implications for clinical practice. J Clin Psychiatry 2014; 75(1): 8-14.
- Beblo T, Sinnamon G, Baune BT: Specifying the neuropsychology of affective disorders: clinical, demographic and neurobiological factors. Neuropsychol Rev 2011; 21(4): 337-359.
- Knochel C, et al: Cognitive and behavioural effects of physical exercise in psychiatric patients. Prog Neurobiol 2012; 96(1): 46-68.
- Greer TL,et al: Dose-dependent changes in cognitive function with exercise augmentation for major depression: results from the TREAD study. Eur Neuropsychopharmacology 2015; 25(2): 248-256.
- Imboden C, et al: Aerobic exercise as add-on treatment improves alertness in depressed in-patients: preliminary results from a randomized controlled multicentre-trial. European Neuropsychopharmacology 2015; 25(9) Suppl 2: S438.
- Holsboer F, Ising M: Stress hormone regulation: biological role and translation into therapy. Annu Rev Psychol 2010; 61: 81-109.
- Wittert GA, et al: Adaptation of the hypothalamo-pituitary-adrenal axis to chronic exercise stress in humans. Med Sci Sports Exerc 1996; 28(8): 1015-1019.
- Heijnen S, et al: Neuromodulation of aerobic exercise – A review. Front Psychol 2016; 6: 1890.
- Foley LS, et al: An examination of potential mechanisms for exercise as a treatment for depression: a pilot study. Mental Health and Physical Activity 2008; 1(2): 69-73.
- Molendijk ML, et al: Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations (n=9484). Mol Psychiatry 2014; 19(7): 791-800.
- Lucassen PJ, et al: Regulation of adult neurogenesis by stress, sleep disruption, exercise and inflammation: implications for depression and antidepressant action. Eur Neuropsychopharmacol 2010; 20(1): 1-17.
- Kobilo T, et al: Running is the neurogenic and neurotrophic stimulus in environmental enrichment. Learn Mem 2011; 18(9): 605-609.
- Schlittler M, et al: Endurance exercise inceases skeletal muscle kynurenine aminotransferases and plasma kynurenic acid in humans. Am J Physiol Cell Physiol 2016; 310(10): C836-40.
- Schuch FB, et al: The effects of exercise on oxidative stress (TBARS) and BDNF in severely depressed in-patients. Eur Acrh Psychiatry Clin Neurosci 2014; 264(7): 605-613.
- Eyre HA, Papps E, Baune BT: Treating depression and depression-like behavior with physical activity: an immune perspective. Front Psychiatry 2013; 4: 34.
- Rethorst CD, et al: Pro-inflammatory cytokines as predictors of antidepressant effects of exercise in major depressive disorder. Mol Psychiatry 2013; 18(10): 1119-1124.
- Hatzinger M, et al: Electroencephalographic sleep profiles in treatment course and long-term outcome of major depression: association with DEX/CRH-test response. J Psychiatric Res 2004; 38: 453-465.
- Breslau N, et al: Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 1996; 39(6): 411-418.
- Passos GS, et al: Effects of moderate aerobic exercise training on chronic primary insomnia. Sleep Med 2011; 12(10): 1018-1027.
- Rethorst CD, et al: Does exercise improve self-reported sleep quality in non-remitted major depressive disorder? Psychol Med 2013; 43(4): 699-709.
- Imboden C, Hatzinger M: Neurobiological basis and evidence of exercise in depression. NeuroTransmitter 2016; 27(10): 40-45.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(4): 25-29.











