Cardiovascular disease ( CVD) is the leading cause of death worldwide. Lowering the level of LDL cholesterol (LDL-C) in the blood reduces the risk of CVD such as heart attacks and strokes. An international group of researchers conducted the largest observational study to date in Europe examining changes in lipid-lowering therapy (LLT) and the achievement of risk-based LDL-C targets according to the 2019 ESC/EAS guidelines for dyslipidemia.
Despite a decline in age-adjusted mortality from cardiovascular disease over the past 40 years, there are still more than 18 million deaths from CVD worldwide each year, a large proportion of which are due to atherosclerotic cardiovascular disease (ASCVD). The Global Burden of Disease Study from 2019 found that high low-density lipoprotein (LDL-C) cholesterol levels are the second largest contributor to disability-adjusted life years lost worldwide, with an estimated 98.6 million life years lost.
In 2019, the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) updated their joint guidelines and recommended stricter LDL-C targets, especially for those at high (<1.8 mmol/l) and very high (<1.4 mmol/l) risk. In addition to appropriate diet and lifestyle, drug treatment to lower LDL-C levels is a proven strategy to prevent both first-time and recurrent ASCVD events. However, recent studies have shown that most patients’ LDL-C levels are still above optimal levels, partly due to suboptimal medication.
Professor Dr. Kausik K. Ray from the Imperial Centre for Cardiovascular Disease Prevention, ICTU-Global, Imperial College London, and colleagues conducted the prospective, observational and descriptive SANTORINI study in patients at high and very high cardiovascular risk in 14 European countries within 2 years of the publication of the ESC/EAS guidelines to assess the implementation gap [1]. The main objective of the one-year follow-up was to assess changes in lipid-lowering therapy (LLT) and achievement of risk-based targets for LDL-C at 12 months compared to baseline. Cardiovascular events during follow-up were assessed as a secondary objective and death from any cause as an exploratory endpoint. Baseline and 1-year follow-up data were collected from patient records from visits related to lipid control where the patient was examined by a physician.
Patients aged 18 and over with high or very high cardiovascular risk were included in the study. Of all 14 participating European countries, most patients were recruited from Germany (23.6%), Italy (21.8%) and Spain (11.1%).
Combination therapy achieved better LDL-C control
Of the 9559 subjects, follow-up data were available for 9136 (2626 at high risk and 6504 at very high risk) and LDL-C data at baseline and follow-up were available for 7210 (2033 at high risk and 5173 at very high risk). Lipid-lowering therapy was increased in one-third of patients and maintained unchanged in two-thirds.
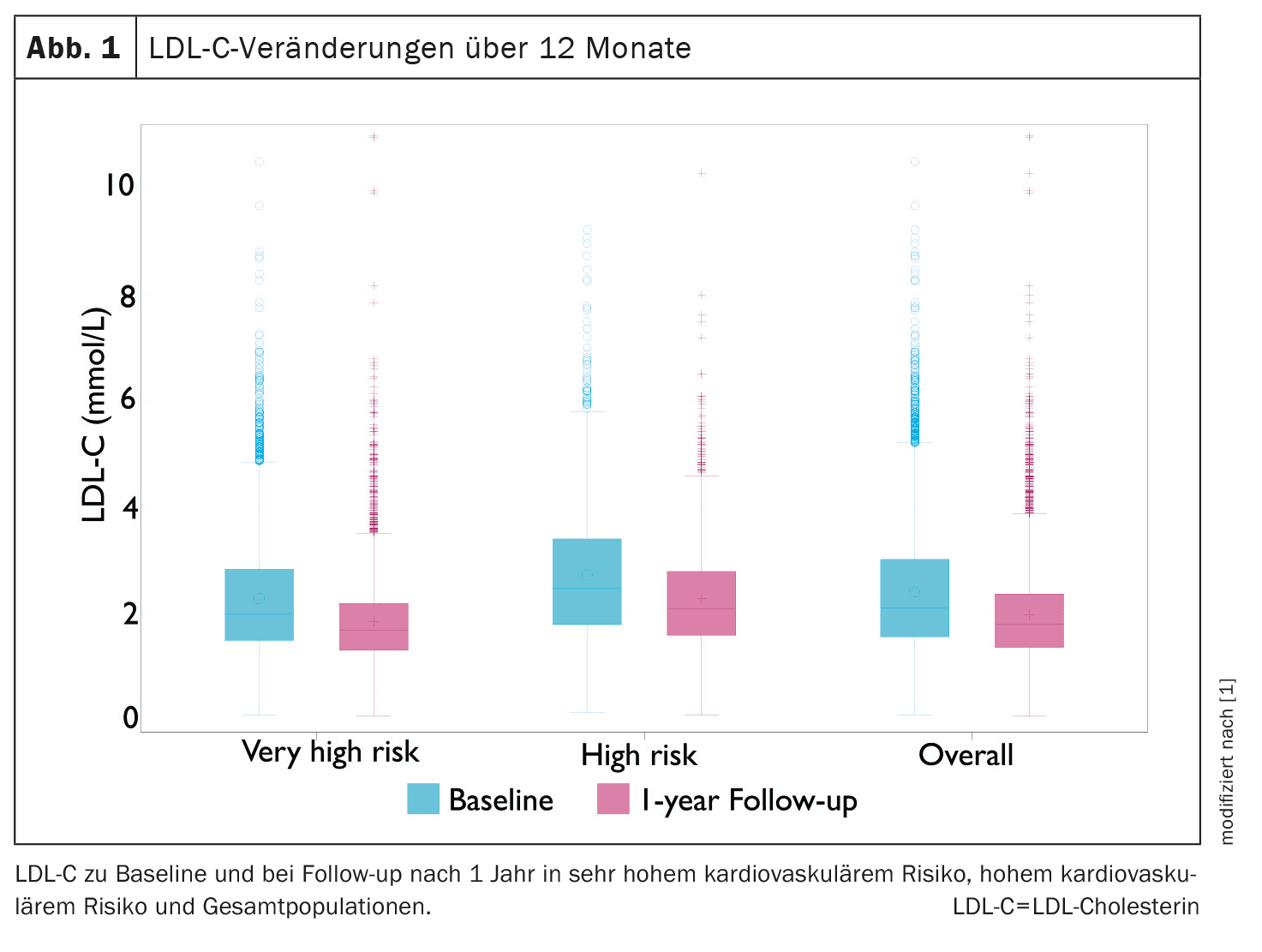
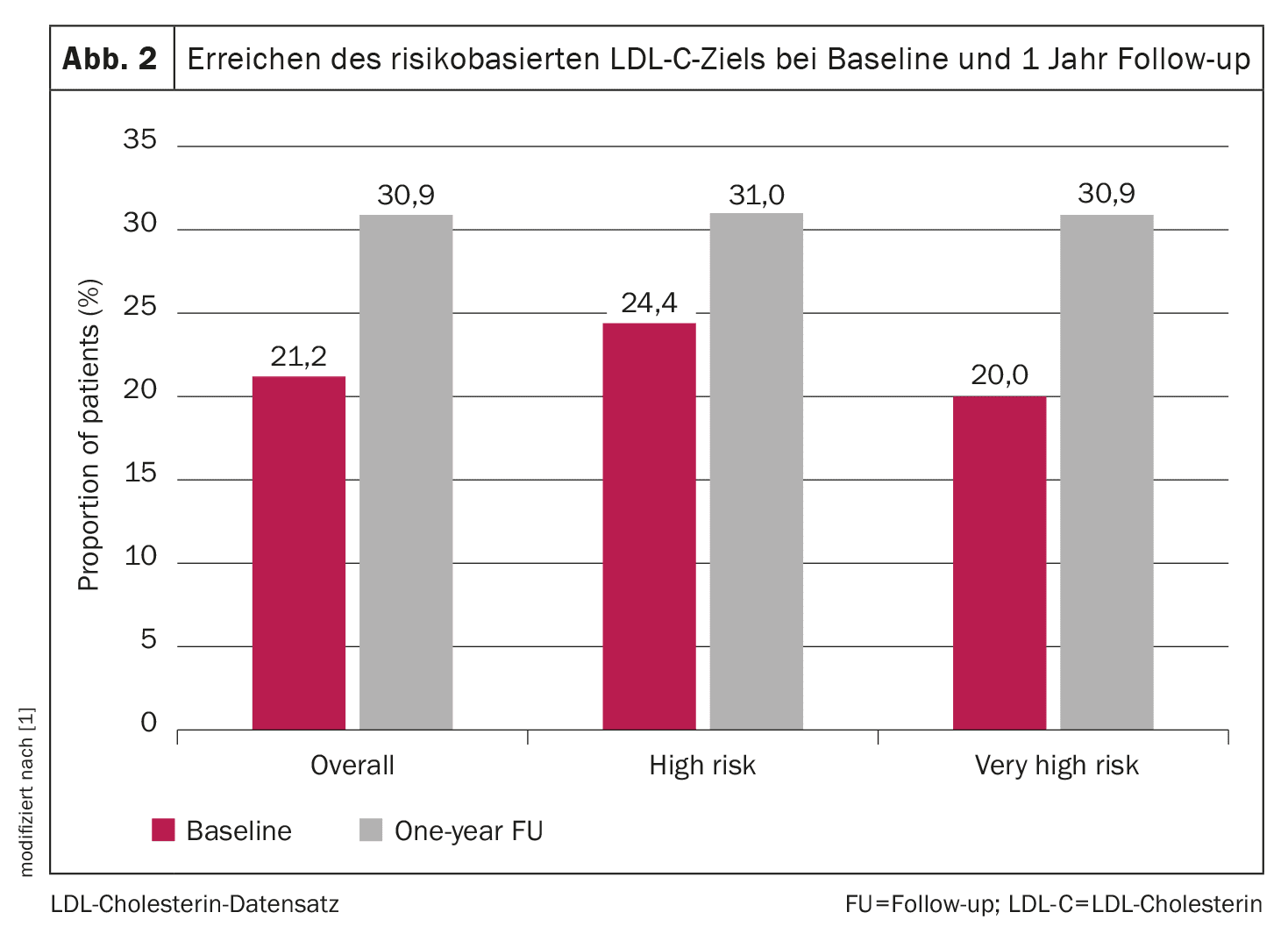
The use of monotherapies and combination therapies increased from 53.6% and 25.6% to 57.1% and 37.9% respectively. Average LDL-C levels decreased from 2.4 to 2.0 mmol/l (Fig. 1). Target achievement improved from 21.2% to 30.9%, mainly due to the use of LLT in those who had not received such treatment at baseline (Fig. 2). In addition, goal attainment was higher with combination therapy compared to monotherapy during the follow-up period (39.4% vs. 25.5%). These results are consistent with previous data suggesting that combination therapies improve the achievement of LDL-C targets.
Despite improvements in the implementation of LLT, the average LDL-C values in patients at high and very high risk were around 0.4 to 0.5 mmol/l above the respective risk-based LDL-C target values. The intensification of treatment during the follow-up period mainly took the form of oral combination therapies with the addition of ezetimibe to statins. In patients who did not receive LLT at baseline, the achievement of LDL-C target after one year was higher in those on combination therapy compared to all monotherapies. It is worth noting that LLT therapies were not intensified in two-thirds of patients during the follow-up period, the authors write.
Prof. Ray et al. also note that there was no obvious explanation for the proportionally higher use of oral combination therapies over a one-year period in those who did not receive LLT at baseline. With the exception of higher LDL-C levels (3.5 vs. 2.2 mmol/l), demographic characteristics and health conditions were generally similar. The moderate intensification of treatment during the one-year follow-up may indicate that there is no urgent need to optimize LLT in asymptomatic patients. In addition, some patients experienced escalation of LLT after a non-fatal MACE, possibly indicating the lack of risk perception in otherwise asymptomatic patients, leading to delays in LLT optimization.
In addition, the treatment approaches for patients with and without ASCVD differed during the follow-up period. For example, the use of statin monotherapy, statin and ezetimibe combination therapy and PCSK9i combination therapy increased by 1.8%, 10.8% and 1.9%, respectively, in patients with ASCVD, while the corresponding figures for patients without ASCVD were 8.0%, 4.2% and 1.7%, respectively. The authors explain that although most demographic characteristics were similar, fewer patients with ASCVD were treated in primary care in the SANTORINI study. In summary, these data suggest that intensification of LLT in patients with ASCVD occurred more frequently in secondary care and with the addition of ezetimibe to statin therapy.
Most patients remained above the target value
Patterns of care in the European countries generally mirrored the overall results, with the vast majority of those not receiving LLT at baseline initiating it and generally more likely to use combination therapies within a year. Nevertheless, the use of combination therapies at the end of the follow-up period varied widely, from 7.1% in the UK to 55.0% in Italy. In terms of risk-based goal attainment, it was lowest in France and Germany, where only about 23% of patients reached LDL-C goal, highest in Austria at 43.9%, and no country achieved more than 50% of patients with target LDL-C levels.
LDL-C levels in high and very high risk patients improved by approximately 0.4 to 0.5 mmol/l, suggesting that at the population level the risk of cardiovascular events would be relatively reduced by approximately 10% to 11%. However, the high and very high risk groups were still 0.4 to 0.5 mmol/l above their respective target values, meaning that a further 10-11% risk reduction would be possible if the LLT targets were achieved.
Despite the observed increase in the intensity of LLT therapies over one year (mostly due to the addition of ezetimibe to statins), two thirds across Europe remained above the risk-based targets. Cardiovascular events in high- and very-high-risk patients also remained high. However, more patients achieved their LDL-C targets when using combination therapies. Therefore, an approach to better implement combination therapies for the majority of patients is warranted at an early stage to better control LDL-C in high and very-high risk patients.
Literature:
- Ray KK, et al.: Use of combination therapy is associated with improved LDL cholesterol management: 1-year follow-up results from the European observational SANTORINI study. European Journal of Preventive Cardiology 2024; 31(15): 1792–1803; doi: 10.1093/eurjpc/zwae199.
CARDIOVASC 2024; 23(4): 41–42
HAUSARZT PRAXIS 2024; 19(12): 22–23