The WHO estimates that there are around 200 million cases of viral pneumonia worldwide every year (not including COVID-19), half of which affect children. In adults, around 20% of all pneumonias are caused by viruses, and the risk is particularly high in older people over 70. In addition to the “usual suspects”, certain risk groups can also be affected by rare pathogens.
Common pathogens of viral pneumonia are influenza, SARS-CoV-2 and RSV. “A healthy adult very rarely catches a pathogen outside of this spectrum,” stated Dr. Michael Knappik, Department of Respiratory and Pulmonary Diseases, Vienna Health Association, Penzing Clinic, Vienna (A) [1]. In such cases, immunosuppressed patients whose immune system is compromised are therefore particularly affected. “On the other hand, there are also regions of the world where rare viral diseases are endemic and can lead to severe infections even in immunocompetent people.” Dr. Knappik went into detail about some of the rare pathogens.
Viral pneumonia with immunosuppression
The most common risk factors are organ transplantation (HSCT/SOT), HIV (depending on CD4 status) and immunomodulatory drugs. Pathogens that can attack such vulnerable patients include CMV, HSV, varicella, EBV, bocavirus, human rhinovirus and adenovirus. “Many of these pathogens lead to normal cold infections in immunocompetent adults and possibly to an exacerbation of an infection in asthma or COPD patients, but very rarely only to pneumonia,” explained the expert.
CMV pneumonia: CMV pneumonia is particularly feared after organ transplantation and in HIV patients with very advanced infection (CD4 <50 cells/μl), said Dr. Knappik. A CT thorax is used for diagnosis, and histopathology is also considered the gold standard to differentiate between a CMV infection or a disease with organ manifestations, for example. However, patients are often in a critical condition, which is why practitioners tend to be reluctant to perform invasive diagnostics and do not want to run the risk of bleeding. Alternatively, quantitative PCR has also proven to be effective (BAL >104-5 cop/ml).
In the initial phase, when the patient is still unstable, ganciclovir 5 mg/kg i.v. q12h is used parenterally. However, valganciclovir 900 mg q12h also has very good oral bioavailability, so that the patient can be switched to it after stabilization, explained the infectiologist.
In the hemato-oncology field, there are occasionally patients who are refractory despite this therapy and in whom an increasing or at least non-decreasing viral load is observed. Maribavir has been available for such cases since 2022, showing a significant improvement in this patient group.
Viral pneumonia with a history abroad
The MERS (Middle Eastern Respiratory Syndrome) coronavirus, which was the second coronavirus to lead to a major outbreak after SARS-CoV-1, is still one of the rare pathogens with a history abroad. Transmission is mainly via camels, less frequently via bats. However, the incidence has fallen massively in recent years: in 2023, there were only two confirmed cases globally, which is why MERS-CoV is now almost negligible.
Hantavirus: Hantavirus can cause Hanta (cardio-)pulmonary syndrome (HPS/HCPS ). Hantaviruses belong to the Bunyaviridae, there are about 20 human pathogenic species worldwide. The annual incidence is around 200 cases worldwide, around 30 of them in the USA alone. Transmission takes place via aerosols (feces, urine, carcasses) from rodents and animal bites. The incubation period is relatively short at 14 days (7-30 days); the primary diagnostic method is PCR.
The so-called Old World hantaviruses lead to nephritis epidemica or fever with renal syndromes and are mainly found in Europe and Asia. In terms of incidence, they are the global leaders, but there are about 15 different hantaviruses in the new world, all of which can lead to cardio-pulmonary syndromes, Dr. Knappik explained.
The early symptoms of HPS are rather unspecific and include fever, myalgia and gastrointestinal symptoms. Cough, bilateral infiltrates, pulmonary edema and ARDS only occur in later stages. Laboratory tests show elevated leukocytes and hemoglobin as well as thrombocytopenia. There is no specific therapy available, “but it has been shown that mortality can be reduced if patients are connected to ECMO at an early stage”. However, with a mortality rate of 40%, the prognosis is still relatively poor.
Nipah virus: The Nipah virus belongs to the Paramyxoviridae, it has an incidence of around 200 cases per year and an incubation period of 4-14 days. Here too, diagnostics are carried out via PCR (ELISA). The virus is mainly transmitted by fruit bats, which feed on fruit and release the pathogen via blood, saliva and urine. People can become infected via contaminated fruit and then spread the virus from person to person. The same applies to pigs.
The Nipah virus is widespread in India and Bangladesh, with a single outbreak in Malaysia at the end of the 1990s. The mortality rates in these areas are over 70%. At the beginning, the symptoms are also rather unspecific with influenza-like (fever, headache) symptoms, later respiratory symptoms also occur. About 3-14 days after these, neurological symptoms (encephalitis) typically occur with dizziness, seizures and coma, which is often fatal in the end.
There are no meaningful therapeutic studies. Remdesivir has been shown to be active in vitro in animal studies, “but this must first be investigated in greater depth,” said Dr. Knappik.
Avian influenza A (H5N1): Influenza A (H5N1) was first described in 1996, but there has not yet been a major outbreak in humans. However, in the last 10 years alone, there have been 9 different new human pathogenic viruses that have been transmitted from poultry to humans. In most cases, these were only a few isolated cases and there were no human-to-human transmissions. 8 of the 9 outbreaks took place in China.
In 2020, a new variant of H5N1 emerged via reassortment, which is a combination of H5N8 and H5N1 and is very effective at transmitting between poultry and between poultry and wild birds. As a result, the first detection in Latin America occurred in the fall of 2022, and in October of the same year a mink farm in Spain with 50,000 animals was affected. Here, mammal-to-mammal transmission occurred, with the minks often dying of respiratory infections. In general, there is increasing evidence in mammals, said the expert, including predators such as foxes, bears and leopards, but also pets such as cats and dogs.
“In poultry, bird flu is not actually a respiratory disease, but rather a gastrointestinal one. However, when dead wild birds are eaten by predators, infections occur, which have also led to mass deaths of seals in the Antarctic, among other things.” In an outbreak among cats in Poland in 2023, the virus also entered the animals via their food.
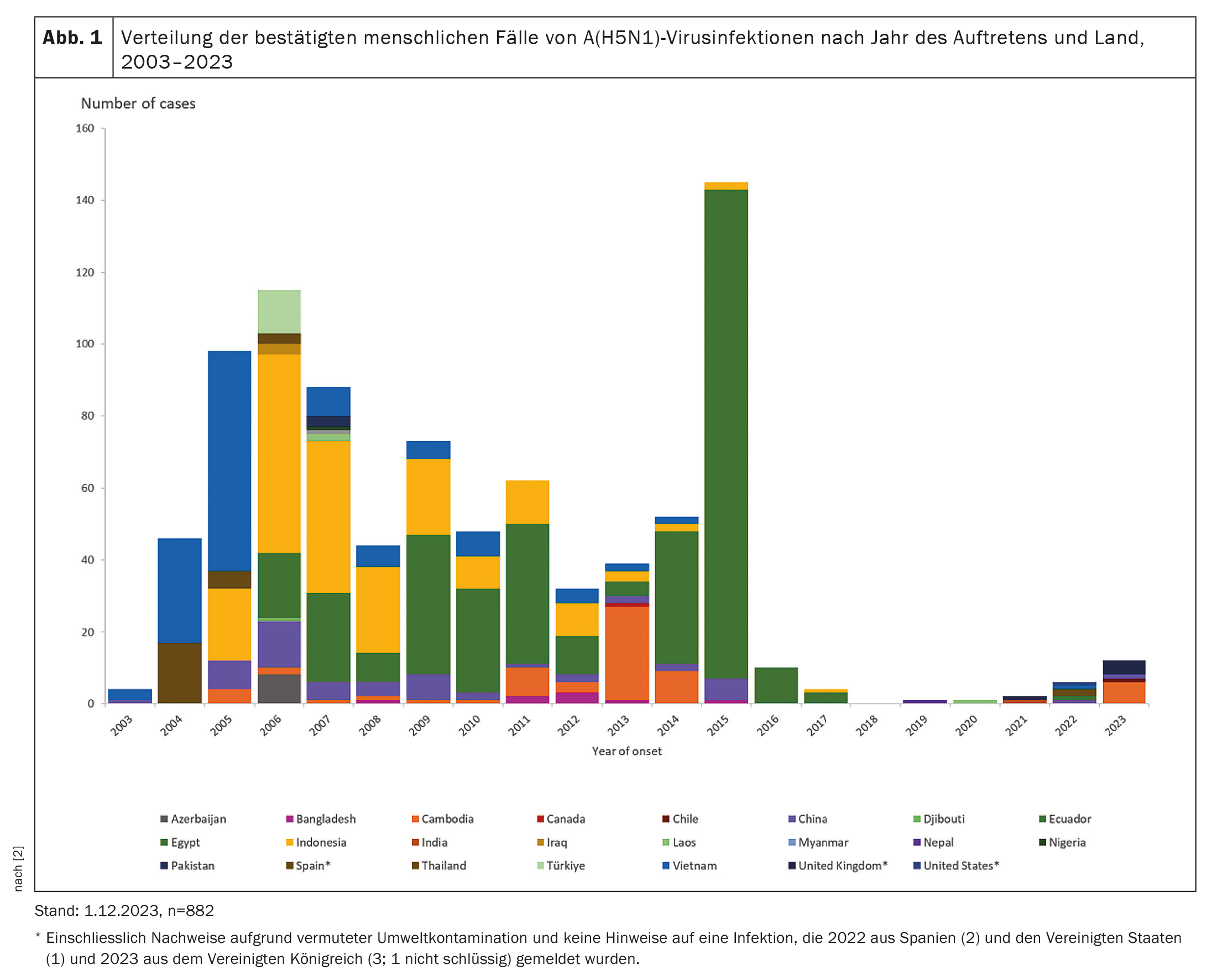
In humans, we can look back on around 20 years of experience and around 880 registered cases of H5N1 (Fig. 1) . The case fatality rate ( CFR) is high at 50%, although human-to-human transmission has not yet been observed, as mentioned above. The new clade does not appear to be as pathogenic and transmission to humans is difficult: despite the sharp increase worldwide, only a few human pathogenic cases are known to date. The WHO also still classifies the current clade as having a low pandemic potential.
Congress: WATL 2024
Sources:
- Knappik M: Lecture “Pneumology goes viral – rare pathogens of viral pneumonia”. 8th Congress of the Scientific Association for the Therapy of Lung Diseases (WATL). Digital, 13.01.2024.
- Adlhoch C, Fusaro A, Gonzales JL, et al: Avian influenza overview September-December 2023. EFSA Journal 2023; 21(12): e8539; doi: 10.2903/j.efsa.2023.8539.
InFo PNEUMOLOGIE & ALLERGOLOGIE 2024; 6(1): 30-31 (published on 6.3.24, ahead of print)