Nephrolithiasis and gout are diseases with an increasing global burden and often co-occur with type 2 diabetes mellitus. SGLT2 inhibitors, which were first approved for the treatment of hyperglycemia in type 2 diabetes mellitus, have shown many cardiometabolic and renal benefits. By increasing urine flow through osmotic diuresis, they may reduce the risk of kidney stones. However, there is limited data on the recurrence of nephrolithiasis in people with coexisting gout.
The incidence and prevalence of kidney stones has increased over the years, with an associated high recurrence rate as well as complications (such as urosepsis), hypertension and permanent kidney damage. As surgery is often required to remove the stones, healthcare costs are also increasing significantly.
Gout is a common and strong independent risk factor for kidney stones, as is type 2 diabetes mellitus. SGLT2 (sodium-glucose cotransporter-2) inhibitors have been shown to have many positive effects on cardiometabolism and renal metabolism. In addition, randomized controlled trials have shown that SGLT2 inhibitors also reduce serum uric acid levels by increasing uric acid excretion, which also translates into a lower risk of gout attacks. Thus, the ability of SGLT2 inhibitors to increase urinary flow and uricosuria may influence the risk of kidney stones, although possibly in opposite directions.
Dr. Natalie McCormick of the Rheumatology and Allergy Clinical Epidemiology Research Center, General Hospital, Boston, and colleagues used target trial emulation to evaluate the recurrence of nephrolithiasis in people with type 2 diabetes who began treatment with an SGLT2 inhibitor compared to patients who initially took a glucagon-like peptide-1 (GLP1) receptor agonist, another second-line glucose-lowering agent. Another group took a dipeptidyl peptidase-4 (DPP4) inhibitor, which served as an alternative comparator [1]. Primary target trial emulation was performed in all patients with nephrolithiasis. In secondary target trial emulations, these patients were stratified according to pre-existing gout at baseline and those without nephrolithiasis at baseline were also included.
Recurrence rates with SGLT2i were lower than with GLP1-RA
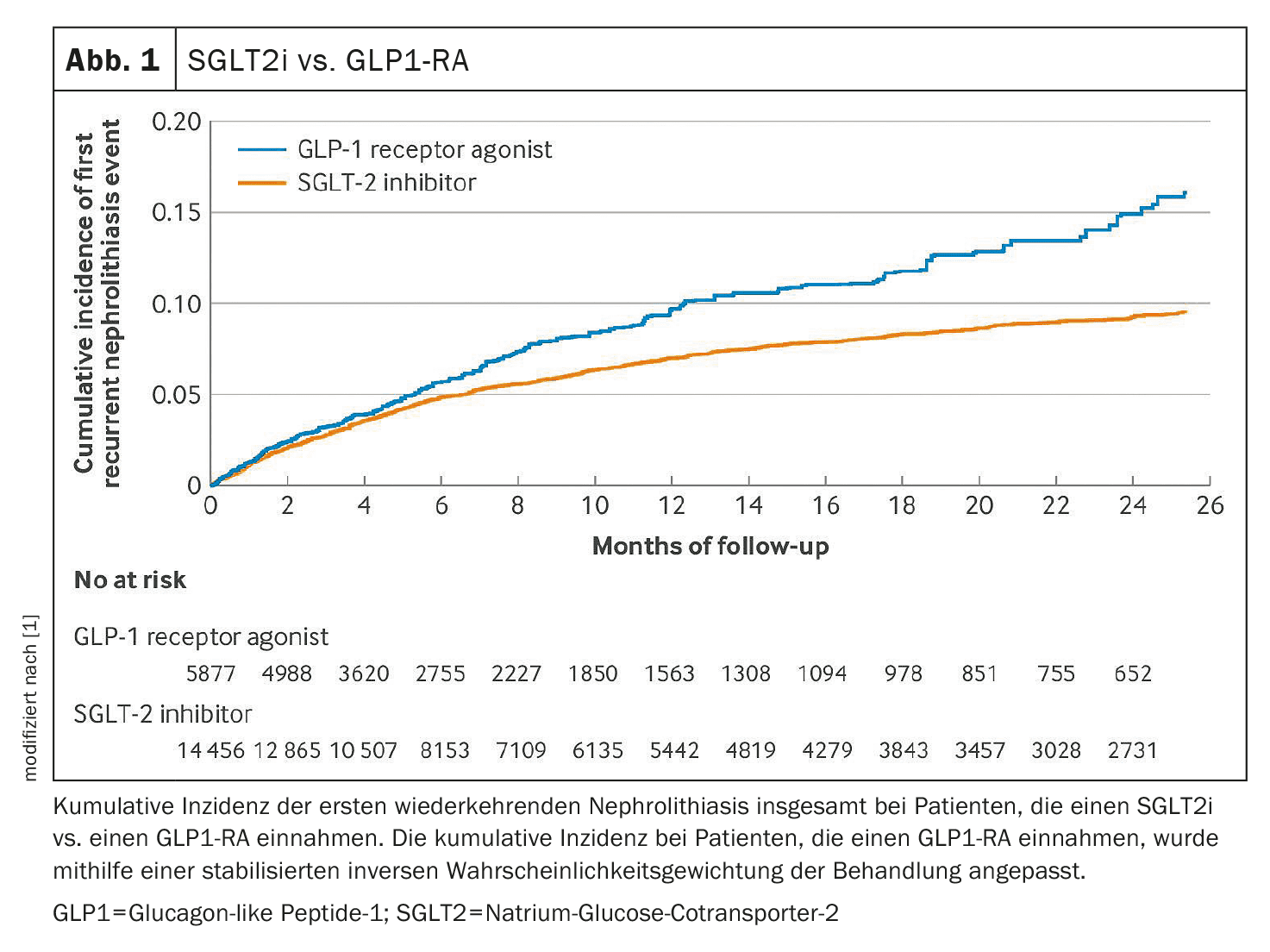
From January 2014 to June 2022, the study included 20,146 patients from the Canadian Population Database with nephrolithiasis and type 2 diabetes, including patients with concomitant gout during the study period. After inverse probability weighting and balancing of all baseline covariates including obesity (standardized differences <0.1), 14456 subjects under SGLT2i and 5877 subjects under GLP1-RA were included in the target study.
The primary outcome was recurrent cases of nephrolithiasis identified by diagnoses during emergency department visits, hospitalizations or outpatient visits. Secondary outcomes included nephrolithiasis leading to hospitalization or emergency department visits and exacerbation of gout, as well as positive (genital infections) and negative control outcomes (osteoarthritis and appendicitis). In addition, Poisson and Cox proportional hazards regression models (primary analyses) and overlap weighting were applied.
In the 14,456 weighted patients using an SGLT2 inhibitor, 1924 recurrent nephrolithiasis events occurred (105.3 per 1000 person-years), compared with 853 events in the 5877 weighted patients taking a GLP1 receptor agonist (156.4 per 1000 person-years). This benefit corresponded to an absolute risk reduction of 51 fewer active nephrolithiasis events per 1000 person-years overall (number needed to treat, NNT, = 20) and 219 fewer nephrolithiasis events in people with recent active nephrolithiasis (NNT=5) (Fig. 1). A similar reduction in rate ratio (RR) was observed in people with concomitant gout, with a reduction in recurrent gout (i.e. double the additional benefit beyond diabetes).
Protective associations persisted for nephrolithiasis events requiring emergency department visits, hospitalization or treatment, and when an SGLT2 inhibitor was compared with a DPP4 inhibitor (RR 0.73, rate difference -38 per 1000 person-years (NNT = 26)). The protective associations also persisted in patients with nephrolithiasis and concomitant gout, with an RR of 0.67 and a rate difference of -53 per 1000 person-years vs. a GLP1 receptor agonist (NNT=19) and RR 0.63 and RD -62 per 1000 person-years vs. a DPP4 inhibitor (NNT=16), respectively. The use of SGLT2 inhibitors was associated with a lower rate of gout attacks (RR 0.72, RD -16 per 1000 person-years) compared to GLP1-RA (RR 0.65, RD -21) compared to DPP4 inhibitors.
Benefit for the simultaneous treatment of recurrent nephrolithiasis and gout
The benefits in nephrolithiasis vs. GLP1-RA persisted in secondary, sensitivity and subgroup analyses, including in patients taking thiazide diuretics (a therapeutic agent for nephrolithiasis) and in nephrolithiasis events requiring an emergency department visit or hospitalization or treatment. The same was true when comparing the use of an SGLT2 inhibitor with a DPP4 inhibitor. The absolute risk reduction tended to be greater in patients with concomitant gout at baseline (compared to DPP4 inhibitors) and was even greater in patients with recent nephrolithiasis, the authors write.
In addition, SGLT2 inhibitors showed a higher risk of genital infections but, as expected, were not associated with an increased risk of osteoarthritis or appendicitis compared to GLP1 receptor agonists. The results were similar when propensity score overlap weighting was applied. According to Dr. McCormick and colleagues, the benefits associated with the SGLT2 inhibitor in nephrolithiasis in target-trial emulation suggest that this class of drugs may be a useful adjunct to current nephrolithiasis treatments, particularly in patients with existing indications (e.g., type 2 diabetes mellitus, heart failure, chronic kidney disease), to simultaneously address recurrence of nephrolithiasis and comorbidities, including gout.
In patients with the additional risk factor of co-existing gout, the use of SGLT2 inhibitors was associated with a concomitant reduction in the risk of a gout attack, with a trend towards a greater absolute reduction in the risk of recurrence of nephrolithiasis (particularly compared to DPP4 inhibitors) given the high background rate. The authors emphasize that these data suggest that SGLT2 inhibitors may be useful drugs in this clinical context of multimorbidity with gout, in addition to their proven cardiovascular and renal benefits.
Their target trial emulation showed that taking an SGLT2 inhibitor was associated with a lower recurrence of nephrolithiasis compared to a GLP1-RA or DPP4 inhibitor. A similar reduction in rate was also observed in patients with co-existing gout, with a concomitant reduction in gout recurrence (i.e. two additional benefits over and above the established diabetes treatment).
Take-Home-Messages
- Nephrolithiasis and gout are common, recurrent conditions with an increasing global burden of disease, often occurring in conjunction with type 2 diabetes mellitus.
- SGLT2 inhibitors, which were first approved for the treatment of hyperglycemia in type 2 diabetes, have been shown to have multiple benefits for cardiometabolism and renal function.
- The use of SGLT2 inhibitors was associated with a lower recurrence of nephrolithiasis than the use of a GLP1-RA, with an NNT of 5 in patients with recent active nephrolithiasis.
- The recurrence of gout was also lower in SGLT2i users with concomitant gout (i.e. double the additional benefit beyond diabetes).
- For patients with an existing indication, an SGLT2 inhibitor may be a useful adjunct to current nephrolithiasis therapies to simultaneously treat recurrent nephrolithiasis and comorbidities, including gout.
Literature:
- McCormick N, et al: Comparative effectiveness of sodium-glucose cotransporter-2 inhibitors for recurrent nephrolithiasis among patients with pre-existing nephrolithiasis or gout: target trial emulation studies. BMJ 2024; 387: e080035; doi: 10.1136/bmj-2024-080035.
FAMILY PHYSICIAN PRACTICE 2024; 19(12): 26-27